Claim Submission Queue
Claim Submission Queue
Clearinghouse Schedule for sending Claims to the Payers
- On most mornings, Claims that are Clearinghouse Accepted are batched and forwarded to the Payers at 10:00 AM. (This is not a guaranteed submission time.)
- If Claims batches are received by 1:00 PM Eastern, all Clearinghouse Accepted Claims will be forwarded to the Payer that same day.
- Claim Batches that are received after 1:00 PM Eastern will be sent the next day.
- Claims will not be sent on weekends or national holidays.
- At least 24 hours before an observed holiday, there will be a message posted to the Help Center Home Page with instructions on timely submissions for Claims.
Access the Claim Submission Queue
The Claim Submission Queue can be accessed from the Home Dashboard (if pinned) and from Claims on the Left Side Menu.
Use this Queue to batch your Claims and to work Claims that did not batch.
A segment only shows if there are Encounters in that Status:
- Encounters with the status of Ready to Batch will be on the list. They can be batched by selecting the Batch Claims button.
- If there are Encounters that will not batch, they will be listed with a Description stating why the claim(s) did not batch.
- Below are some examples of claims that will not batch but are not limited to these:
- New/Retired Providers: Any Encounter that has a billing provider with a New or Retired Status in the Provider Library.
- To send Claims, the Provider's status must be set to Active in the Billing/Rendering Provider Library.
- Open Reference Batch: Encounters that are in an Open Reference Batch will not be batched until the Reference Batch is Closed.
- Zero Balance: Encounters that have a zero balance.
- If the Zero-Balance Encounter still needs to be sent to the Payer, change the Status to on the Encounter to Ready for Submission/Resubmission.
- This allows the claim to be sent with a zero balance.
- Example: The Primary Payer Pays in full, but you want to send it to the Secondary even with a zero balance.
- If the claim should not be sent, change the Encounter status to Finalized Paid.
- Encounters can be held from claim submission for a defined number of days using the Hold Claim feature in the Procedure Code Library.
- Encounters with this status have not reached the defined number of days.
- Encounters can be held from claim submission for a defined number of days using the Hold Claim feature in the Service Facility Library.
- Encounters with this status have not reached the defined number of days.
- Credit Balance: Encounters with this status have a credit balance and are not in the Claim Status IP06.
- Held Due to Credentialing: One or more Providers on the Claim(s) are being held for Provider Credentialing.
- Held Due to Tags: Claim(s) have Tags that are preventing them from batching.
- Adjudication Unbalanced: The Adjudication of the Primary Insurance Payment must balance before the Secondary Insurance can be submitted.
- Payment + Adjustments + Patient Responsibility = Charge Amount.
- This also applies to the Secondary Adjudication when being sent to the Tertiary Payer.
Work the Claims that did not Submit
The Encounters are organized by the issue that is preventing them from batching. Review and correct all Encounters from one place.
Select the number link in the Encounters column to navigate to the Claim Submission Queue screen.
Use the Filter Criteria
The Filter Criteria can be used to Close a Reference Batch, find Encounters and Billing Provider Claims. You can also search by Description.
Close a Reference Batch from the Claim Submission Queue Screen
- Select the Green button in the Reference Batch column to close the batch.
- To display all Encounters in the Reference batch before closing the batch, select the number in the Reference Batch column.
- After reviewing the Encounters, close the Reference Batch by selecting the Opened Status on the Title Bar.
Send Zero-Balance Encounters/Credit Balance Encounters
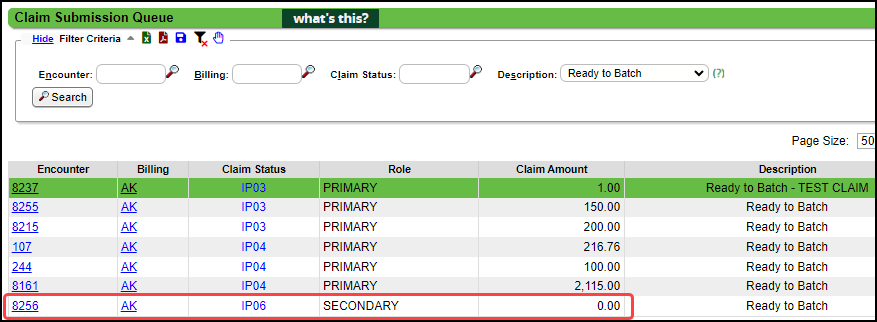
When Claims are not batched because of a Zero or Credit Balance, they will appear in the Claims Submission Queue as Zero Balance (IP06) and Credit Balance.
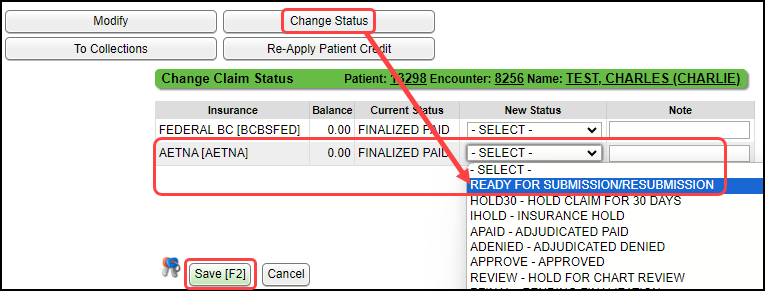
- Using the Change Status button on the Encounter Dashboard, select the Status, Ready for Submission/Resubmission on the Insurance being sent the zero balance Claim.
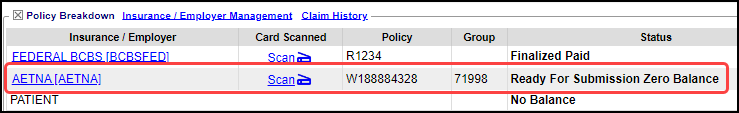
- The Status will display on the Encounter Dashboard as Ready for Submission Zero Balance (IP06).
- If the Status for an Encounter that has a Credit Balance, the Status will display as Ready for Submission.
- Change it to Ready Submission/Resubmission.
- The Status on the Credit Balance Encounter Dashboard will change to Ready for Submission Zero Balance.
- Once the Status is changed, the Claims will appear in Ready to Batch in the Claims Submission Queue.
Learn More
Clearinghouse Rejections
Rejection Examples
Payer Rejections
Claims Management Dashboard
Claim History
Charge/Claim FAQs
Rejected Claims on the Encounter by Status Panel
Related Articles
Claim FAQs
Claims Stuck Why are Claims stuck in the status of Ready for Submission? Claims are stuck in Ready for Submission Examples: The most common reason is that the Reference Batch is not closed. It will be listed in the Claims Submission Queue as Open ...Claims Management Dashboard
Claims Management Dashboard Claims Management Dashboard Overview Claims can be manually batched and uploaded at any time, or the Job Scheduler can be used to automate the Claims batching and upload process at a pre-set day and time. Close the ...Claim Batch History
The Claim Batch History screen shows a list of all Claim Batches that have been created. Select Claims on the Left Side Menu. In the Claim Submission Queue panel, select the Claim Batch History link. Claim Batch History 1-2 Filter Criteria: Use the ...Unbalanced Claims
A common rejection is for Unbalanced Claims: Payments and Adjustments do not equal Charges. If an Encounter is unbalanced or missing the Primary Insurance adjudication, the Claim will not batch. The Primary Payment on the Claim must be posted ...Manually Batch and Upload Electronic Claims
Manually Batch Claims Go to the Claims Management Dashboard by selecting Claims on the Left Side Menu. Ready to Batch In the Claim Submission Queue panel, select the Batch Claims button. To view the Individual Claims, select the number in the ...