Medicaid TPL/Carrier Code
Send TPL/Carrier Code on Medicaid Secondary Claims
Overview
TPL: Third Party Liability; Some Payers refer to this as a Carrier Code, not to be confused with CFI
State Medicaids may require the TPL/Carrier in different places in ANSI Loop 2330B and can be different for each Payer address.
- Use the TPL ANSI Field Group to add the TPL/Carrier Code.
- This will need to be added on the Modify Charge screen on each Claim.
- It will output in Loop 2330B, REF segment or 2330B, NM109 segment depending on the State Medicaid.
- Use a Cross Code (contact support for setup)
- This is set up on the Primary Payer and is only done once.
- Depending on the State, the System will put the TPL in the Segment where it belongs. (2330B Loop, NM109 segment or 2330B Loop, REF segment)
ANSI Field Groups
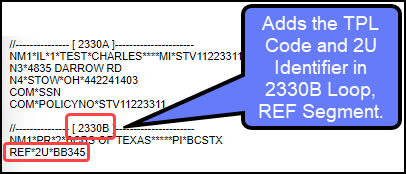
- Example 1: Illinois Medicaid requires the TPL in Loop 2330B in the REF02 segment with a 2U Identifier.
- Use the ANSI Field Groups to populate the TPL with the 2U Identifier on the MCDIL Secondary Claims.
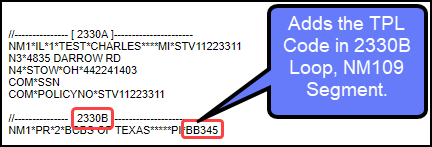
- Example 2: Massachusetts Medicaid requires the TPL in Loop 2330B NM109 segment. This replaces the Payer ID on MCDMA Secondary Claims.
Payers: TPL/Carrier Code Required in Loop 2330B REF Segment with 2U Identifier
- Illinois Medicaid
- Arizona Medicaid
- SC Medicaid
Payers: TPL/Carrier Code required in Loop 2330B NM109
- Massachusetts
- Vermont
- https://dvha.vermont.gov/sites/dvha/files/documents/providers/Forms/GeneralProviderManual.pdf
- https://www.vtmedicaid.com/assets/hipaaTools/TechSpecs_5010/837ProfTechSpecs-5010.pdf pg 30
- http://www.vtmedicaid.com/#/manuals.
ANSI Field Groups
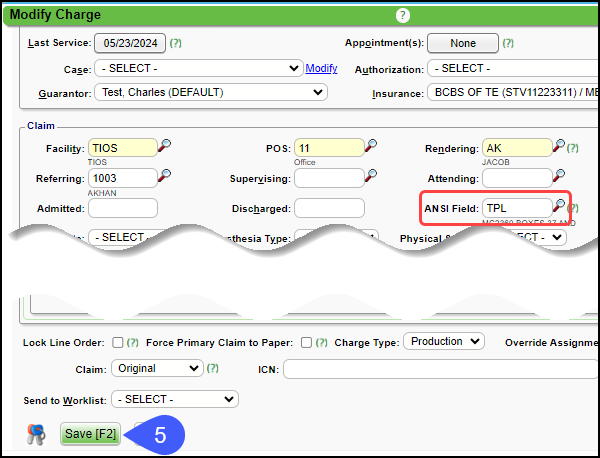
- On the Encounter Dashboard, select the Modify button.
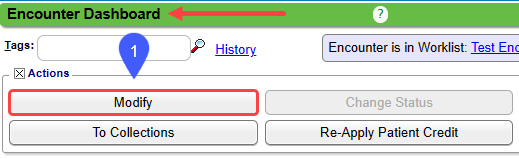
- Using the Lookup icon, select TPL.
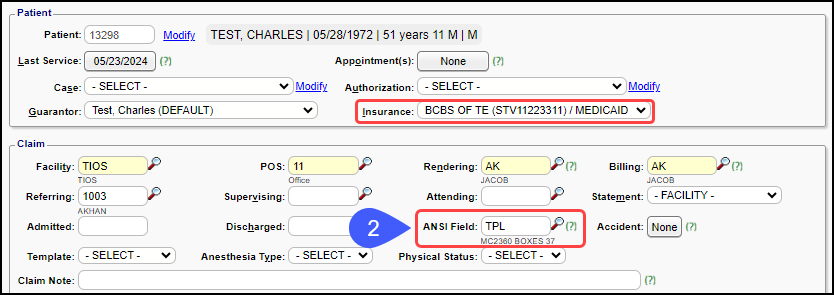
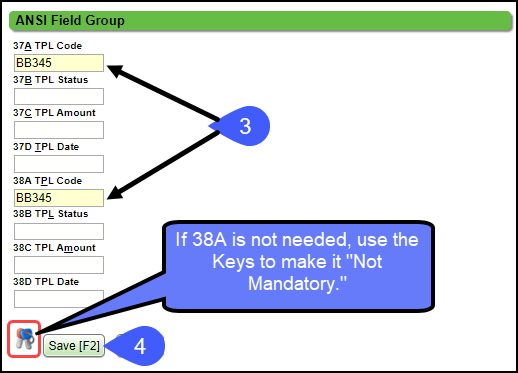
- ANSI Field Group pop-up:
- Enter TPL code in boxes 37A and 38A.
- Select Save [F2].
If you don't need box 38A, select the Keys icon to set the field to Not Mandatory.
- Select Save [F2] on the Modify Charge screen.
Send Additional Information
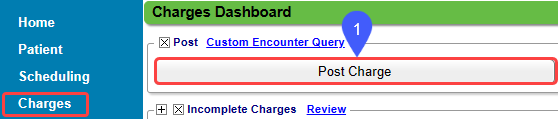
- From Charges on the Left Side Menu, select the Post Charge button.
- Select TPL in the ANSI field. Learn More: Illinois Medicaid TPL Code
- 37A: TPL Code
- 37B: TPL Status
- 37C: TPL Amount
- 37D: TPL Date
- 38A thru 38D are the same as above for additional TPL information.
- The TPL information displays on the paper (HCFA) Claim and on the Electronic Claim in ANSI Loop 2330B.
Related Articles
Add/Modify/Delete Transaction Codes
The System delivers pre-defined Transaction Codes for Payments, Adjustments, Write-Offs, Transfers, and Collections, which cannot be changed by the User. You are not limited to the pre-defined Transaction Codes. System delivered Codes in the ...Reorder/Delete Diagnosis Codes
When Charges are created from the Clinical Documentation or when reviewing Charges, the Diagnosis Codes may need to be reordered before billing the Claim. Diagnosis Codes can be reordered or deleted easily in the Diagnosis panel on the Add/Modify ...Add/Modify a Procedure Code (CPT)
CPT® Codes (Current Procedural Terminology) is a uniform medical language that defines the Procedures or Services performed by a qualified healthcare professional. They are referred to in the System as CPT or Procedure Codes. Adding fees directly to ...Billing/Rendering/Referring Provider FAQs
Add a Provider How do I add a Provider? Providers are added in Libraries: Billing/Rendering Providers Referring Providers/PCP Billing/Rendering and Referring Providers Import Tool Provider Numbers Where do I add the Provider's Medicaid number? ...Patient Types and Patient Codes
Patient Types and Patient Codes Patient Types and Patient Codes There are two ways in Patient Demographics to flag Patients: Patient Type Patient Code Patient Type and Code can be used together or used separately to identify Patients who meet certain ...
