Provider Level Adjustments on the ERA
Adjustment/Payment made at the Provider Level
There are times that the Insurance has a Takeback, Penalty, Interest, or other Adjustments at the Provider Level.
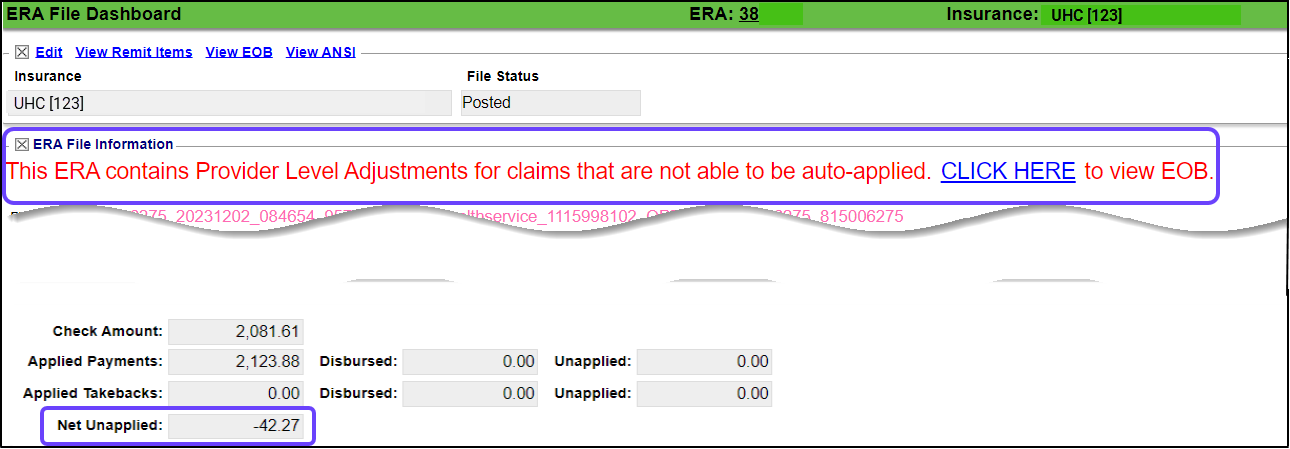
- The Provider Level Adjustments are notated in bold red letters on the ERA File Dashboard.
- These amounts must be manually posted.
- The notification may indicate that the Provider Level Adjustment will be taken in the future on another Remit and should not be posted on the current Remit.
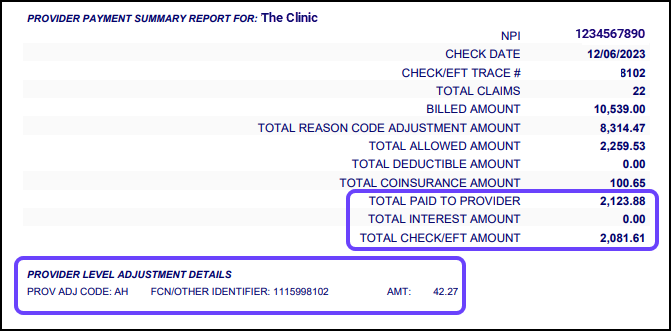
Near the bottom of the EOB, there will be a section giving additional details.
- If the Total Paid to Provider is more than the Total Check/EFT Amount, it is an indication that the Provider Level Adjustment was taken. (The difference between the two should be the Provider Level Adjustment Amount.)
- If the Total Paid to Provider is less than the Total Check/EFT Amount, the Provider Level Adjustment was not taken. It is a notification that the Provider Level Adjustment will be taken on a future Remit. (The difference between the two should be the Provider Level Adjustment amount.) See Future Takeback Notification.
Post the Provider Level Adjustment
- One of these methods can be used to post the Payment/Adjustment.
- Attach a New Receipt to post the Payment/Takeback or other Adjustment;
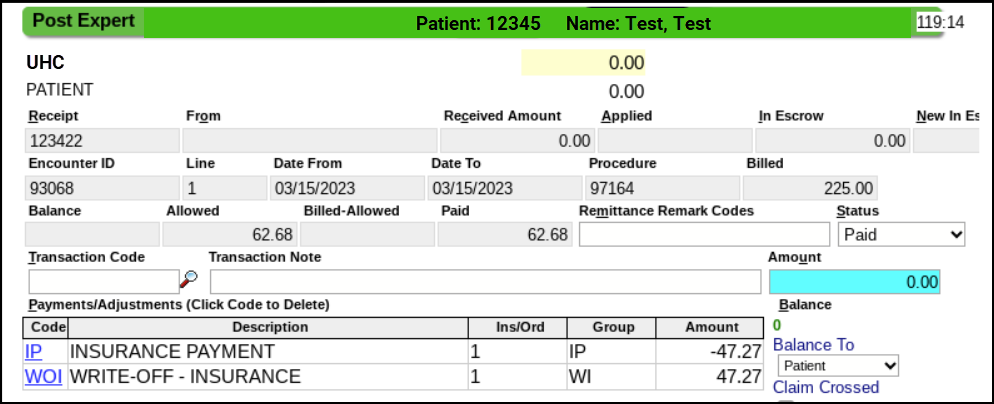
- Use Post Expert on the ERA to post to a specific Patient on the Remit; or
- Create a "dummy" Patient with a "dummy" Encounter with a zero dollar Fee.
- If Post Expert is chosen, use Transaction Code, IP, entering a negative amount if the money is being taken; use positive amount if the Payer is paying you extra money.
- Use a Write-Off Transaction Code, such as WOI, to offset the Payment/Adjustment amount.
Post Expert Example
Change the Receipt Amount to $0.00
If the Future Takeback is the only Transaction on the ERA, you may need to change the Receipt amount to $0.00.
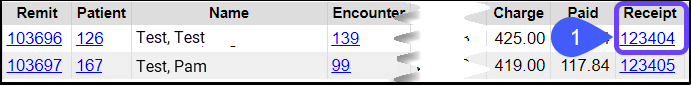
- On the ERA Remit Items screen, select the Receipt number.
- On the Receipt Dashboard, select the Modify link.
- Enter 0.00 in the Received field.
- Select Save [F2].
- Return to the ERA Remit Items by selecting the link at the top of your screen.
- Select the Remit number.
- Update the Remit Status from On Hold to Posted or add to a Worklist or assign a Tag to the Encounter.
- Select Save [F2].
What is an AH Adjustment on a Remit?
An AH Adjustment is a Claim Transmission Fee Amount as a Provider Level Adjustment.
- This code is used for transmission fees that are not specific to or dependent upon individual claims.
Learn More
Post Interest or Penalty
Related Articles
ERA Management Profiles, Rules, and CARC Crosswalk
Use caution when changing ERA Rules. Test updates with relevant ERAs when possible, and closely monitor ERA application after adding, modifying, or removing any ERA Management Rules. ERA Management Profiles, Rules, and CARC Crosswalk Overview ERA ...Post a Zero ERA Payment with a Takeback
If the Remit has a Zero Dollar Payment, but it has Payments in the body of the Remit, there are probably Takebacks at the bottom of the Remit, which results in a Provider Level Adjustment. If the Payments in the body of the Remit equal the Takebacks ...Manage ERAs from the ERA List Screen Using Filters
To access the ERA List screen, from Payments on the Left Side Menu, select the All ERAs link on the Payments Dashboard. All ERA categories can be managed from this screen. Filter Criteria Use the Filter Criteria to qualify which ERAs to view. ...ERA Takeback/Refund/Reversal
Post as Remitted vs. Using the Takeback Process Using Post as Remitted on the ERA completes a Takeback exactly as the Remit dictates in the ERA. In some cases, the Manual Post button will be used to do the Takeback when the ERA does not calculate ...Attach New Receipt to an ERA
This is used when posting Interest, Penalties, Incentive (bonus) Payments or Claim Level Adjustments, such as Takebacks. Create a Receipt for Interest, Penalty, Incentive, or Provider Level Adjustments Select the ERA number. On the ERA File ...