Productivity Analysis Report
Productivity Analysis Report
The Productivity Analysis Report contains Totals for Receipts, Charges, and Applied Payments grouped by specific categories.
Access the Productivity Analysis Report: From Reports on the Left Side Menu, select the Productivity Analysis button.
Receipts Panel
Receipts are totaled by Type of Payment:
- Insurance Payments
- Invoice Payments
- Patient Payments
- Cash
- Check
- Credit
- Total
- Total
- % of Total

- The Receipt Management Report will match the Receipts Panel on the Productivity Analysis Report if run by the same criteria.
- Either Exclude or Include Disbursements on both reports.
The Productivity Analysis Report does not have Refunds included.
- If run by the same criteria, the Practice Analysis Report will balance to the Productivity Report for Charges and Applied Payments.
- Un-posted (Escrow) Receipts are not on the Practice Analysis Report.
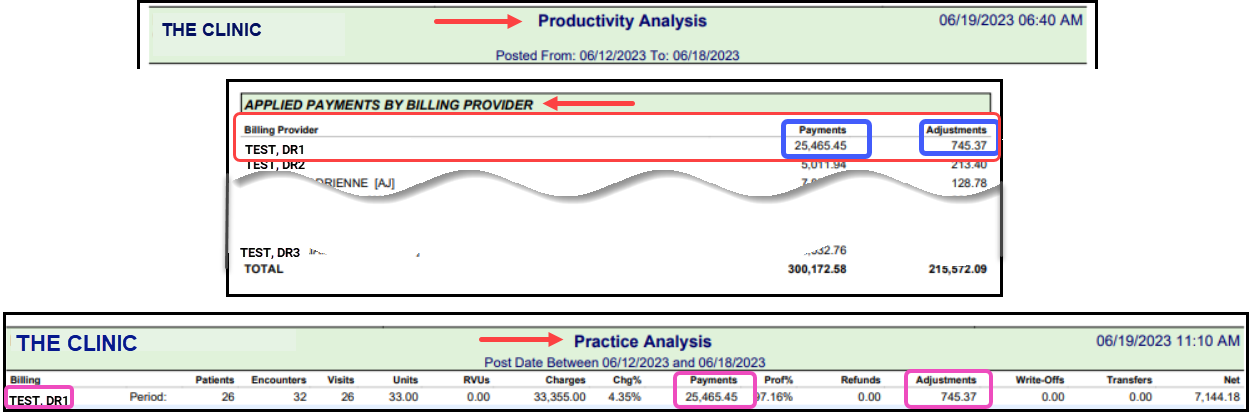
- Example: If the Practice Analysis Report is Grouped by Billing Provider, the numbers for Applied Payments on the Productivity Analysis Report for the Billing Provider will be the same. See screenshots below.
- User the Same Date Range on both reports.
- Select Use Date as Use Charge Post Date on the Productivity Analysis Report. The Practice Analysis Report runs by Post Date by default.
- If Reversed Encounters are Included in the Productivity Analysis Report, the Exclude Reversed Encounters must remain unchecked on the Practice Analysis Report.
- Leave Include Collections unchecked on the Practice Analysis Report.
- Group by Billing Provider on the Practice Analysis Report to match with the Applied Payments by Billing Provider on the Productivity Analysis Report.
Access the Productivity Analysis Report: From Reports on the Left Side Menu, select the Productivity Analysis button.
'Applied Payments & Adjustments by' Panels
- Insurance
- Insurance Reporting Group
- Rendering Provider
- Facility
- Billing Provider
- Collections Payments
If run by the same criteria, the Practice Analysis Report will balance to the Productivity Report for Charges and Applied Payments. These are applied Payments and Adjustments. The Practice Analysis Report does not include un-posted (Escrow) Receipts. The Receipt numbers cannot be compared to the Payments on the Practice Analysis.
- Example: If the Practice Analysis Report is Grouped by Billing Provider, the numbers for Applied Payments on the Productivity Analysis Report for the Billing Provider will be the same. See screenshots below.
- User the Same Date Range on both reports.
- Select Use Date as Use Charge Post Date on the Productivity Analysis Report. The Practice Analysis Report runs by Post Date by default.
- If Reversed Encounters are Included in the Productivity Analysis Report, the Exclude Reversed Encounters must remain unchecked on the Practice Analysis Report.
- Leave Include Collections unchecked on the Practice Analysis Report.
- Group by Billing Provider on the Practice Analysis Report to match with the Applied Payments by Billing Provider on the Productivity Analysis Report.
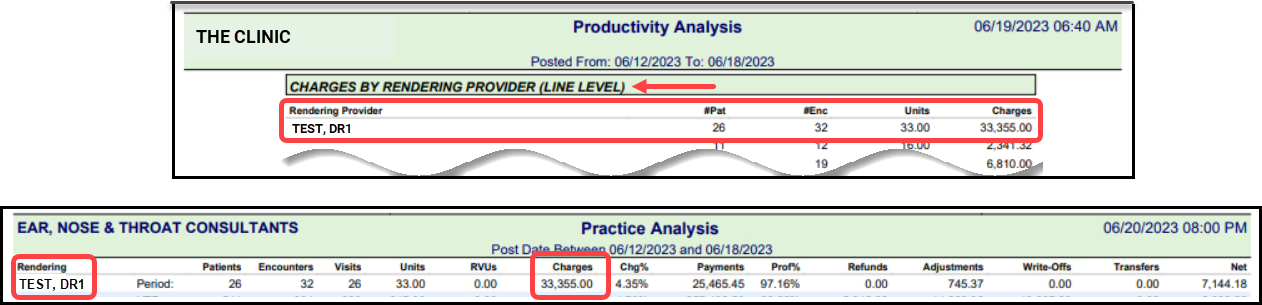
'Charges with #Pat, #Enc, Units, Charges by' Panel
- Rendering Provider
- Insurance
- Insurance Reporting Group
- Facility
If run by the same criteria, the Charges on the Practice Analysis Report will match the Charges on the Productivity Report.
Related Articles
Reports Criteria Overview
Most Reports default to the Post Date which is controlled by the date used in the Reference Batch. My Reports Panel: The Reports that the User has run are shown in this Panel. You can choose to see Unread reports only. Report History: This is the ...Reports Dashboard
Reports Dashboard The Reports Dashboard gives access to the following Reporting Panels: Transactions Financial Patient A/R Scheduling Period End Collections POPS PHI (Protected Health Information) The Reports that contain PHI are labeled with this ...Payroll Report
Note: The Payroll Report cannot be run with a single total. Instead, use the Practice Analysis Report. The Payroll Report calculates the total amount of Revenue generated by a Procedure (displayed by the Procedure Code) for a Provider and reports the ...Referral Source Analysis Report
Referral Source Analysis Report The Referral Source Analysis Report can be used to analyze Patients/Visits that are the result of specific Referring Providers. This information can be pulled from the Referring Provider on the Patient Dashboard or ...Practice Analysis
Practice Analysis This is one of the most used reports in the System due to the output calculations and the ability to create multiple Group By levels. Report Features Date Type allows reporting by Post Date, Date of Service, or on an individual ...