Payroll Report
 Note: The Payroll Report cannot be run with a single total. Instead, use the Practice Analysis Report.
Note: The Payroll Report cannot be run with a single total. Instead, use the Practice Analysis Report.The Payroll Report calculates the total amount of Revenue generated by a Procedure (displayed by the Procedure Code) for a Provider and reports the total Payment that the Provider received.
- Use the Report Filters to isolate specific Providers, Provider Reporting Groups, Procedure Codes, and Procedure Code Reporting Groups.
- Providers are broken down by Type: Billing, Rendering Claim Level, Rendering Line Level.
- Run the Report by Date Type or Date Span.
- Note: The Totals on this Report exclude Refunds.
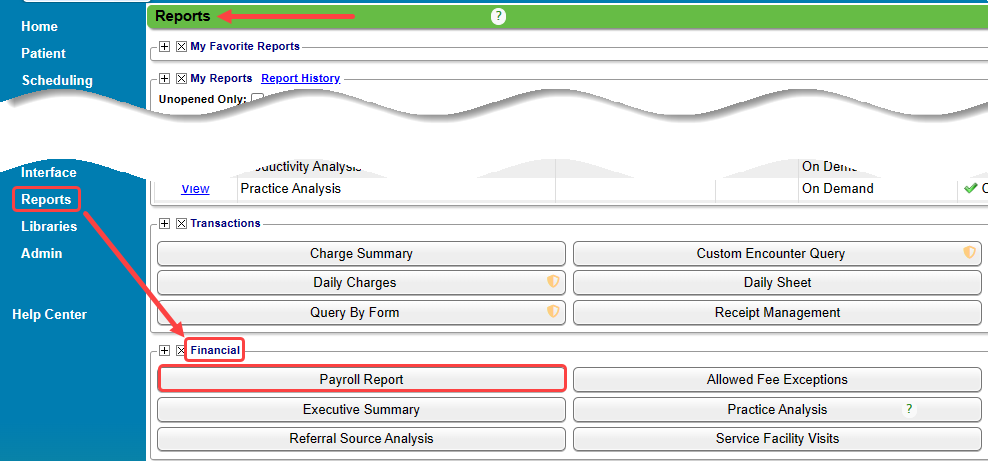
Reports > Financial Panel > Payroll Report
Report Filters
- Provider: Select one or multiple Provider IDs to be used on the Report.
- Provider Reporting Group: Library > Provider Reporting Group
- CPT®: Select one or multiple Procedure Codes.
- CPT® Reporting Group: Library > Procedure Codes
- Insurance: Include or exclude one or multiple Insurances.
- Example: To exclude Patient Payments from the Report, select PATIENT as the Insurance, and toggle the filter to Exclude.
- Insurance Reporting Group: Include or exclude one or multiple Insurance Reporting Groups.
- Percent: Enter the Percent of the Payment that each Provider on the Report will receive.
- The Percent calculates the Provider Payment field: Payment x Percent = Provider Payment.
- A Percent must be entered for the Provider Payment field to populate.
- Show Percent: Displays the Percent (entered in the Percent box) in the Report title.
- Include Previously Paid: Adds a column that displays the sum of the Insurance and Patient Payments that were paid before the current reporting period.
- Include Remaining Balance: Adds a column that displays the remaining balance to be paid.
- Mark Encounters as Paid: Populates the custom field "Payroll Paid Date" with the current date if Use Charges Instead of Payments is checked.
Payment Example
Charges Example
Percent Example
Learn More
Add/Edit a Reporting Group
Use Reporting Groups
Reports Criteria Overview
CPT copyright 2019 American Medical Association. All rights reserved.
Related Articles
Reports Dashboard
Reports Dashboard The Reports Dashboard gives access to the following Reporting Panels: Transactions Financial Patient A/R Scheduling Period End Collections POPS PHI (Protected Health Information) The Reports that contain PHI are labeled with this ...Allowed Fee Exception Report
To find underpayments, this report compares posted allowed amounts to contractual allowed amounts. The Allowed Fee Exceptions Report shows discrepancies on Posted Allowed amounts against the Allowed Fee Schedule. It does not report on CO's and ...Reports Criteria Overview
Most Reports default to the Post Date which is controlled by the date used in the Reference Batch. My Reports Panel: The Reports that the User has run are shown in this Panel. You can choose to see Unread reports only. Report History: This is the ...Productivity Analysis Report
Productivity Analysis Report The Productivity Analysis Report contains Totals for Receipts, Charges, and Applied Payments grouped by specific categories. Access the Productivity Analysis Report: From Reports on the Left Side Menu, select the ...Custom Query Reports Hub
Custom Query Reports (CQR) Custom Encounter Query = CEQ Custom Receipt Query = CRQ Custom Transaction Query = CTQ Custom Patient Query = CPQ Custom Appointment Query = CAQ Overview Filters and Criteria Create a CQR CEQ CRQ CTQ CPQ CAQ Overview Custom ...