Payer Rejection: Readjudication Payer Claim Control Number (ICN)
A6 ACK/RETURNED - REQUESTS FOR RE-ADJUDICATION MUST REFERENCE THE NEWLY ASSIGNED PAYER CLAIM CONTROL NUMBER FOR THIS PREVIOUSLY ADJUSTED CLAIM. CORRECT THE PAYER CLAIM CONTROL NUMBER AND RE-SUBMIT.
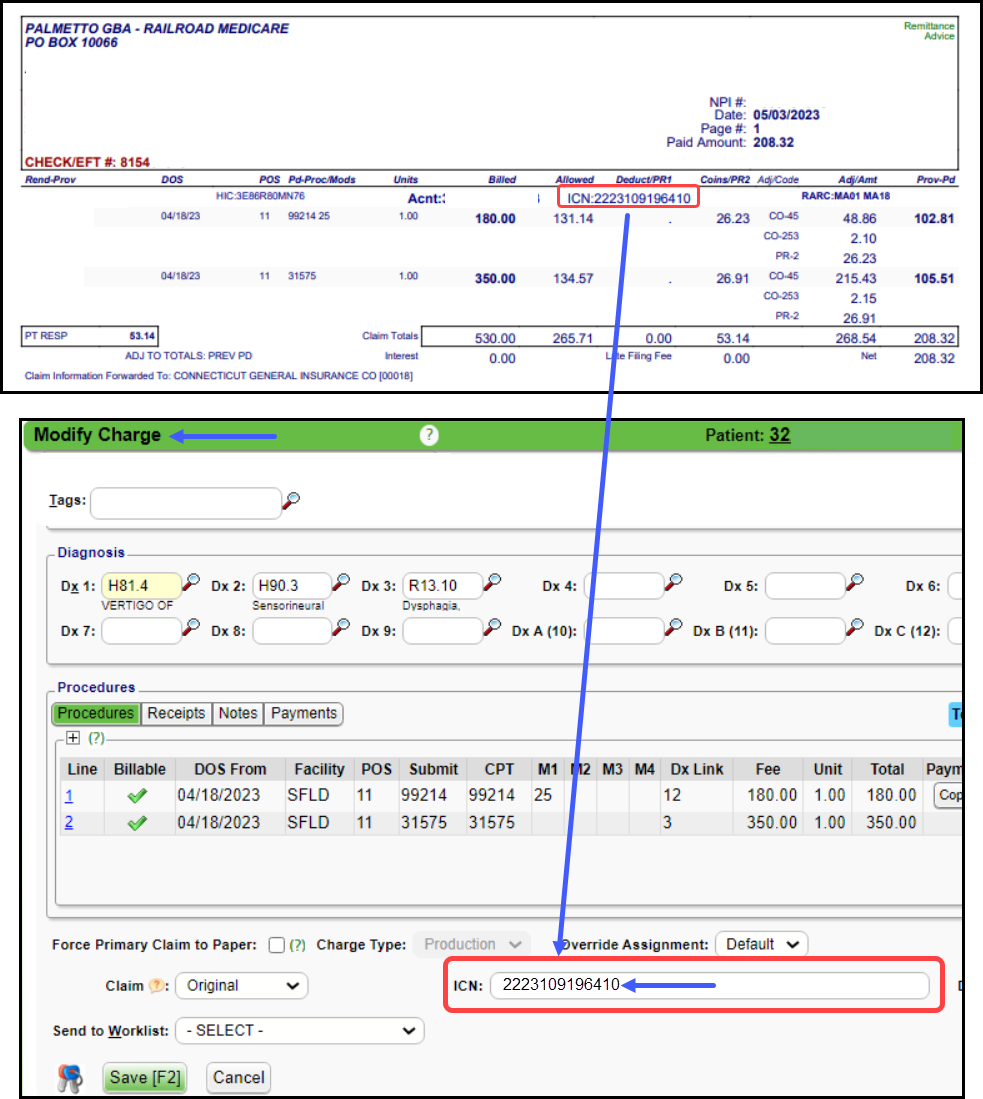
- The ICN Number is missing for a previously adjusted claim.
- Resolution: Find the ICN number on the Remit and add it to the Claim.
Related Articles
Payer Rejection Articles
Payer Rejections Payer Rejections Overview Acknowledgement/Receipt Payer Rejection: A6 -A1-;Acknowledgment/Receipt Adjudication Date Payer Rejected: INVALID ADJ PAYMENT DATE Claim Filing Indicator (CFI) Payer Rejection: INVALID FILING INDICATOR CODE ...ICN (Internal Control Number)
The ICN auto-populates from the most recent ERA posted for this encounter. Expand the Charge panel on the Encounter Dashboard to see if there is an ICN attached. If posted from a Paper Remit: Select the Modify button on the Encounter Dashboard. ...Payer Rejection: Reason Not Clear
Payer Rejection: Reason Not Clear Payer Rejection prefixes: EP: Third-Party Clearinghouse AP: Payer Contact the Payer Payer Rejections can be more difficult to read as they often do not comply with standard responses. For Payer rejections that you ...Claim History
Claim/Encounter History On the Claim Status History screen, you can view Claim Status progression from the start to finish. The oldest date defaults to the bottom of the list, but you can resort by clicking on the column title. On the Encounter ...Send Replacement/Corrected Claim/Delayed Reason/Void
Denial vs Rejection A Denial is a Claim that the Payer has adjudicated but is denying Payment on one or more Charges on the Claim. You have either received a Paper or Electronic Remittance with the denial. Denied Charges can be resubmitted as a ...