Anesthesia Charge Entry
This article highlights the differences in Anesthesia Charge Entry.
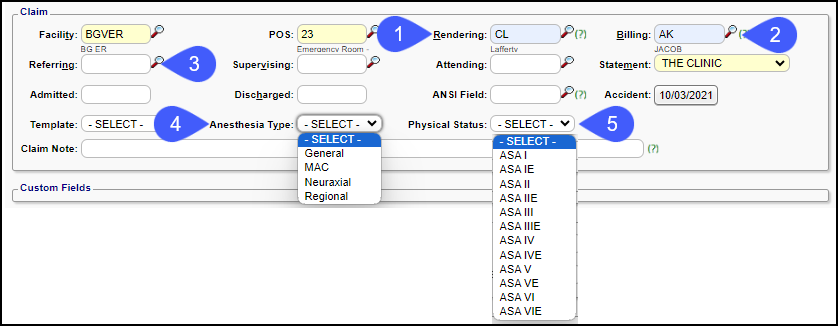
- Rendering: Select the Provider administering anesthesia.
- MD, CRNA, Resident
- Billing: Select the Billing/Supervising provider.
- Usually the anesthesiologist
- Referring: Enter the Surgeon performing the Procedure, if needed.
- Anesthesia Type: Reportable
- Required for AQI reporting
- Can be used to automatically apply a modifier (QS) when the anesthesia type is MAC (Monitored Anesthesia Care)
- Physical Status:
- Reportable
- Required for AQI reporting
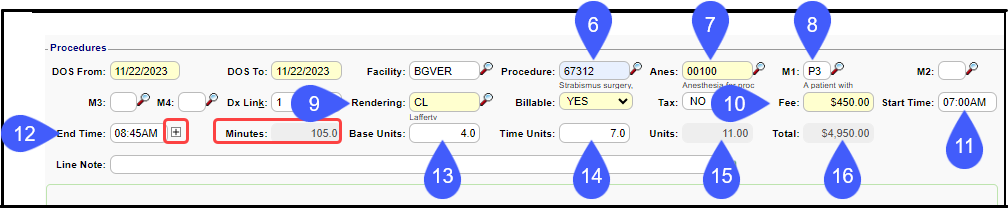
- Procedure: Required field.
- If entering the Surgery code AND the Anesthesia code, the surgery code is entered here.
- If entering Anesthesia codes only, enter the anesthesia code here.
- If the Crosswalk is loaded into Admin > Anesthesia Time Units, the Anesthesia code populates automatically when the Surgery code is entered in the Procedure field.
- If the Crosswalk is not loaded:
- Enter the Anesthesia code ONLY if the Surgical Procedure Code was entered in the Procedure Code field.
- Otherwise, leave blank.
- Enter the Modifiers.
- Physical Status: Reportable
- Required for AQI reporting
- Modifier P3 & P4 can be set up to add units to the base unit count automatically in the Anesthesia Time Units Setup.
- Concurrency Modifiers will be System added later.
- Rendering Provider: The Rendering Provider can change at the Service Line level (CRNAs, Residents, etc.).
- This field will auto populate from the Rendering Provider selection in the Claims panel.
- Change here if the Rendering is different for a specific line item.
- This outputs on electronic claims but not on paper claims.
- Fee: Will auto populate the per Unit rate.
- Enter the Anesthesia Start time
- Enter the Anesthesia End time.
- Exact minutes matter!
- If the Anesthesia service was interrupted:
- Selecting the plus icon opens a window allowing the addition of multiple Start and Stop times.
- The system calculates the minutes for each Start and Stop, and includes them in the minutes field.
- Base Units: The System uses the Base Units set up in the Procedure Code library.
- May also be automatically increased by modifier P3 or P4 per Anesthesia Time Units Setup.
- Example: Procedure Code was set up with Base Units = 3 and Modifier P3 with 1 Unit.
- The Base Unit calculation will be 4.
- Time Units: The System converts the minutes to Time Units based on the Anesthesia Time Units Setting.
- Units: The System totals Units to be billed (base + modifiers + time)
- Total: The System calculates the total Charge amount: Fee x Units
- In the Example: ($450.00 x 11 = $4,950.00)

**NOTE: If other charges, such as Office Visits, are billed in the same database where Anesthesia charges are billed, do not enter the Start and End Times on the non-anesthesia Charges for the Time Units to equal 0.00.**
Learn More
Charge Entry
Anesthesia Time Unit Settings
Anesthesia Visit Concurrency
Anesthesia Medically Directed Modifiers
Anesthesia Billing Resources
Anesthesia Military Time
Related Articles
Anesthesia Time Unit Settings
The Anesthesia Time Unit Settings determine how time is translated into Units. Set up a default that is used for all Payers. If a Payer uses a different (non-default) logic, add a separate Time Unit Calculation Profile and link to that specific Payer ...Anesthesia Billing FAQs
Anesthesia Billing Setup How do I set up Anesthesia Billing? Setup for Anesthesia Billing Anesthesia Billing Resources Anesthesia Billing Resources Resources for Anesthesia Billing Concurrency Why is Anesthesia billed using Concurrency? Anesthesia ...Enter a New Charge (Encounter) Manually
Before entering Charges, attach to a Reference Batch. Close the Reference Batch when finished reviewing the Charges. If the Reference Batch is left open, the Charges will not batch. Accessing the Post (Add/Modify) Charge Screen Use one of the ways ...Anesthesia System Settings
ANESTHESIA ACTIVATES THE ANESTHESIA FUNCTIONALITY A System Setting must be added to use Anesthesia Billing. This setting will activate the Anesthesia Functionality, add a new System Setting Tab, and allow additional customization. (Admin > System ...Anesthesia Visit Coding
Anesthesia Visit Coding is activated in System Settings > Charges > VISITCODING > Yes Users must be able to View Anesthesia Crosswalk to use Anesthesia Visit Coding. Admin > User Maintenance > User ID > Permissions > Admin > Setup > Time Unit ...