Secondary Payer Allows/Pays more than the Primary Payer
Sometimes the Secondary Payer allows more than the Primary Payer allowed.
This most often occurs when the Patient has a private insurance versus a group insurance for the secondary.
- The Secondary Payment is more than the balance.
- Posting the Secondary Payment will leave a credit.
Scenarios
If the Secondary Payer paid as Primary in error, the over payment should be refunded.
If the Secondary Payer has verified that this Payment is correct because of a higher allowed amount, you can reverse a Primary adjustment, and post the Secondary Payment.
Reverse the Primary Adjustment/Post Secondary Payment
Reverse the Primary Adjustment for the same amount as the credit would be if the the Secondary Payment was posted.
- The object is to have a balance of zero when finished.
Example:
- Charge Amount: $250
- Primary Payment: $150
- Primary Allowed: $175
- Primary CO45 Adjustment: $75
- Primary PR: $25
- Balance is $25
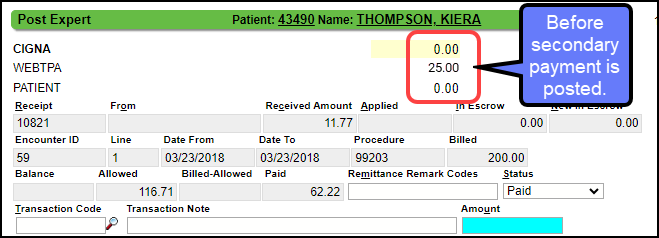
- The Secondary Pays
- Secondary Payment: $50 (There is a balance of $25)
- Secondary Allowed: $200 ($25 more than the Primary Allowed)
- Balance would be -$25 if posted.
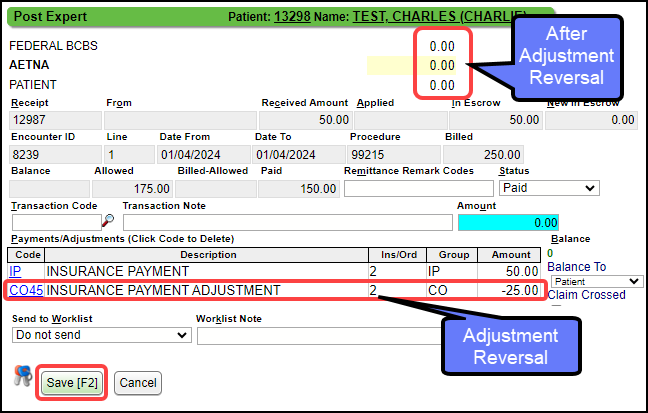
Reverse the Adjustment and Post the Payment
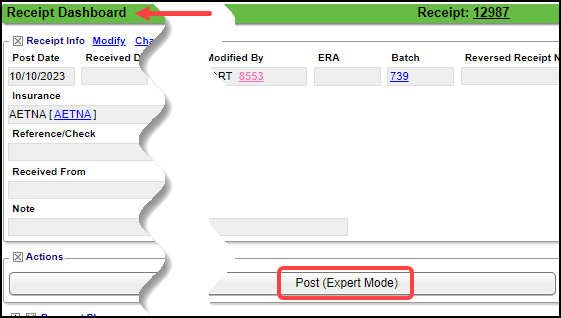
Use Post Expert:
- On the Receipt, select the Post {Expert Mode} button.
- If on an ERA, use Post Expert on the ERA Remittance Screen.
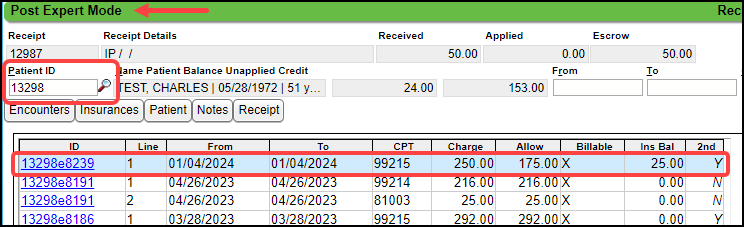
- If the Patient ID is populated, tab.
- If blank, find the Patient or enter the Encounter number preceded by an e (e1234).
- Select the line item where the adjustment needs to be reversed.
- Enter Transaction Code: IP
- Amount: 50.00
- Tab
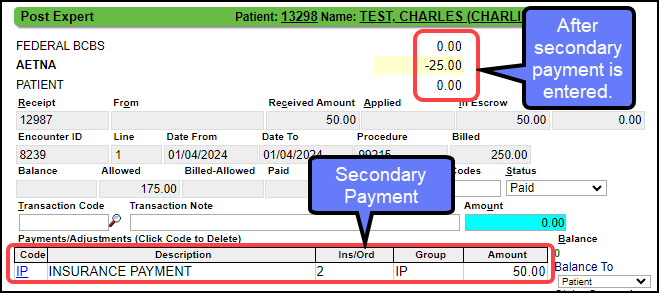
- Enter another Transaction Code: CO45.
- Amount: -25.00 (negative) (Enter the amount that shows as the balance at the top of the Posting screen.)
- Tab (Balance should be $0.00)
- Select Save [F2].
Related Articles
ERA FAQs
ERA FAQs Archived ERAs How do I Archive ERAs? Archive ERAs Update an ERA's File Status Where do I find Archived ERAs? Find Archived ERAs Status Claim Type Why does the ERA Claim Type say it is Processed as Tertiary when the Patient only has a Primary ...Add or Modify Insurances in the Insurance Library
Add or Modify Insurances in the Insurance Library When adding Payers to the Insurance Library, the System automatically creates numeric Insurance IDs unless you have elected to create your own. Create Your Own Insurance IDs Go to Admin on the Left ...Manually Post a Secondary Payment like a Primary Payment
Post a Secondary Payment as you would a Primary Payment Normally, you would not post a CO45 on a Secondary Payment. The Secondary Payment screen does not have the option to enter a CO45. However, there may be an occasion where this is necessary to ...Payer Rejections
Payer Rejections Overview Payer Rejections Overview When a Claim is submitted electronically, the information on the individual Claim is matched with the information the Payer has on file. If the information is not in alignment with the Payer ...Medicare Secondary Payer Reason (MSP)
In order for the MSP code to be sent on a Secondary Medicare Claim, the Medicare Insurance CFI must be set to MB. If Medicare is secondary, this is a mandatory field. If using Eligibility, the MSP will auto-populate. Otherwise, choose the Medicare ...