Complete the Incomplete Charges for Billing
The Incomplete Charges can be individually completed or multiple Encounters can be completed by selecting the checkboxes in the column between Action and Encounter.
- If All the Encounters are selected,
- The ones that don't have errors will complete.
- The ones with errors will show on a Validation popup and will not complete.
- You can also filter by like-kind errors or types of Claims using the Filter Criteria.

Alert: Whenever you Complete one or multiple Incomplete Charges, Copays that have been entered during Appointment Check In/Check Out will auto post to the Encounter.
Complete an Individual Charge for Billing
- Select the checkbox next to the Encounter number.
- Select Complete.
- Validation Warning:
- Confirm by choosing Save & Continue. The Encounter will auto-status to Ready for Submission. When the Reference Batch is closed, this Claim will be batched for submission to the Payer in the next batch of Claims.
- If there is a Validation Error, re-status for Hold or Review before selecting Save & Continue. The Claim will not be batched until the error is corrected.
Complete Multiple Encounters
- To complete multiple Encounters, select the Encounters you want to complete or select all the Encounters using the checkbox on the Columns bar.
- Select the Complete Selected Encounters button.
Validation Warning: When multiple Encounters are being completed together, a Validation Warning displays that indicates the following:
- The number of Encounters that have no errors and will be completed.
- The number and list of Encounters that have Charge Management Warnings with the option to complete or not complete.
- The number and list of Encounters that cannot be completed due to Charge Management Errors.
- The number and list of Encounters in a Global Period.
- At the bottom of the screen, the number of Encounters To be Completed and To Be Reviewed with the ability to Assign Tags is displayed.
- Select Save and Continue.
- A filtered screen will display automatically with the Encounters that were not selected for completion.
- The Encounters that were completed will be Ready for Submission and can be batched after the Reference Batch is closed.
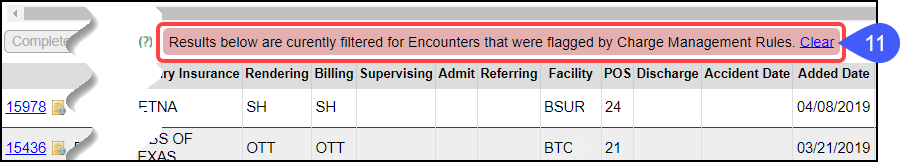
- This filtered screen is indicated by a red banner.
- To return to your original screen, select the Clear link on the red banner.
For the Encounters that were not completed, a banner will display at the top of the Modify Charge screen with the Charge Management Rule and Rule number.
Complete Multiple Incomplete Self-Pay Encounters
This System Setting controls the ability to complete multiple Self-pay Encounters from the Incomplete Charge Review screen.
Example: A Patient is checked-in/checked-out on the Calendar and a Patient Payment is collected.
- This Encounter is Self-Pay.
- The Copay field automatically populated when adding the Payment from the Calendar.
- Since the "Insurance" is "Patient", there is no Copay, but this was not caught during Check-in/Check-out.
- Having an entry in the Copay box prevents the completion of multiple Self-Pay Encounters in one step.
- Each one would need to be completed separately because of the Copay Exception Warning.
- Adding this System Setting will change the Copay field to $0.00 and bypasses the Copay Warning which will allow completion of multiple Encounters.
Learn More
Incomplete Charge Review Overview
Incomplete Charges: Filtering Criteria
Related Articles
Incomplete Charge Review Overview
What are Incomplete Charges? These are Charges that have not been completed to send to the Payer. They are created by: Charges that have been sent from your Chart Documentation System; Charges that are Imported with the Import Tool; or Charges that ...Incomplete Charges: Filtering Criteria
Use Filter Criteria to facilitate your workflow to review and complete a limited subset of Encounters. Examples: A biller/coder only works with Medicare charges, use the Insurance filter. If you only work with a certain Provider(s), use the Billing ...Daily Charges Report
The Daily Charges Report is a detailed breakdown of each Patient's Charges for a day or a date range. This report can be run at the end of the day to capture your Charges, or it can be run for a different period to report Charges and Payments for the ...Billing Resources
While we provide many resources for the best use of the System, sometimes groups need basic training on medical billing, and that is training we do not provide. Resource Suggestions Hire a billing company: If you have recently lost an experienced ...Billing/Rendering Providers
Add Providers Providers can be added individually using the NPPES Import Tool or en masse using the Import Tool. Using the NPPES Import Tool will complete the Provider screen that will only require editing. Using the Provider Import Tool, all ...