Chiropractic Specifics
Specialty Code
- Enter the Specialty Code, 35, in the Provider Library
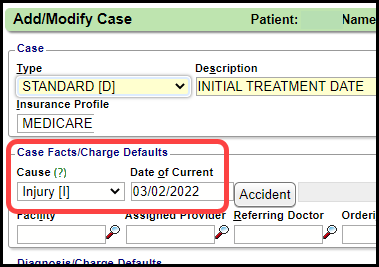
Add a Case
- Create a Case.
- Select the Default checkbox.
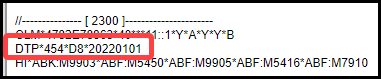
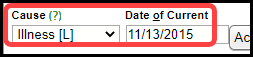
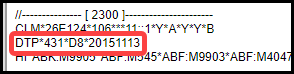
- Cause:
- Injury (I)
- Qualifier 454
- Illness (L)
- Qualifier 431
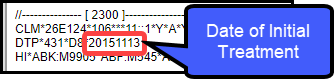
- Date of Current: Date of Initial Treatment (functions the same as DIT ANSI Field)
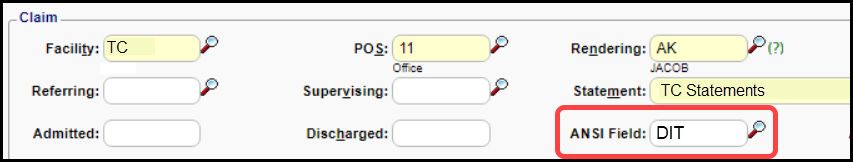
DIT (Date of Initial Treatment) ANSI Field Group
Some groups use the DIT ANSI Field, DIT for adding this data to the claim. This field must be built by Support or your Implementation Manager.
Related Articles
Add/Modify a Procedure Code (CPT)
CPT® Codes (Current Procedural Terminology) is a uniform medical language that defines the Procedures or Services performed by a qualified healthcare professional. They are referred to in the System as CPT or Procedure Codes. Adding fees directly to ...Add a Case and Authorization
Add a Case and Authorization Cases can be added in multiple places in the System. Select this link: Cases and Authorization Overview Add a Case For this example, the Case is added on the Patient Dashboard. Select the Case link on the Patient ...Add a Case for Workers Comp
Workers Compensation Case Cases allow specific information for repeated Charges and Appointments per patient. Workers Compensation Policy The Insurance Profile for Workers Comp should be added first. See Workers Compensation Policy Profile. Add a ...Charges System Settings
Charges ACCIDENTONCASE ENFORCE ACCIDENT IS ALWAYS ON A CASE Mandatory: Always require an Accident on new Cases, for ALL Case Types. Not Mandatory (and ---): Cases will not require an Accident on the Case. Note that it rarely makes sense to set this ...OB/GYN Billing Specifics
Create a Case for Pregnancy Add Last Menstrual Period (LMP) Date Cause: Set to 'P' for Pregnancy. Date of Current: Date of Last Menstrual Period (LMP) These 2 fields will populate the ANSI 2300 Loop. Example: DTP*484*D8*20130205 Learn More Add a Case ...