Jopari Rejections
Jopari, a third-party clearinghouse that handles Workers Compensation Claims, provides Payer Rejections that may not align with typical Payer Rejections.
- The following should be included on Claims that are sent to Jopari:
- SSN
- WC Address
- Authorization
Rejection: Jopari Requires the Patient (Dependent) Loop on all Claims
Reason for Rejection
- The Claim is missing the Policy Holder relationship 20 - Employee.
Fix the Rejection
- From the Encounter Dashboard, under the Policy Breakdown panel, select the Insurance Policy.
- From the Add/Modify Policy window, update the Insured Relationship to 20 - Employee.
- Update the Policy Holder Employer/Attorney field to the correct employer.
- Select Save [F2].
- Resubmit the Claim.
Rejection: Attachment Not Received
If a Payer Rejects stating that the Attachment was not received:
- You have verified in the PWK segment of the electronic Claim that the document was sent, but the Payer insists that it was not received.
- The Payer may be expecting a certain Type of Document, and that type was not sent.
- Ask the Payer the Document Type they are expecting.
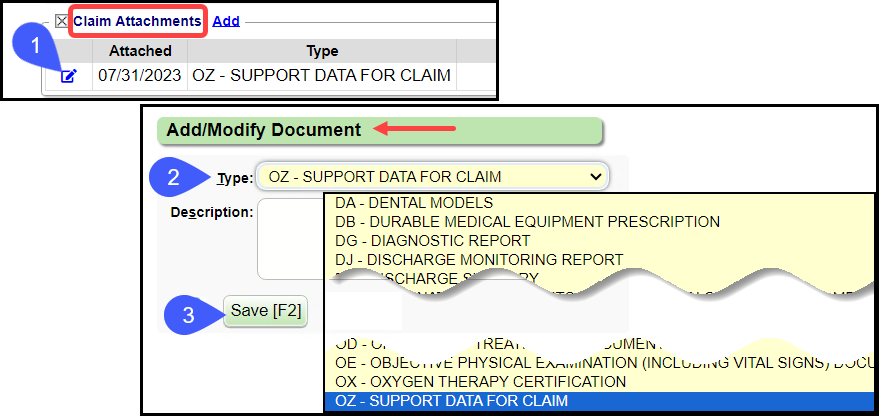
To Confirm or Change the Document Type
- In the Claim Attachments panel on the Encounter Dashboard, select the Edit icon.
- OZ - Support data for claim is the default Document Type that is sent.
- Confirm or change the Document Type that the Payer is expecting using the dropdown.
- Select Save [F2].
Rejection: Patient Eligibility not Found with Entity
Reason for Rejection
There are many reasons that the Payer may not be able to determine the insured status of a Patient. The most common reasons include:
- The Patient's demographic information is not up to date.
- The Payer does not have all of the necessary information about the Patient.
Fix the Rejection
- Call the Payer for Eligibility information (Eligibility, Demographics etc.) and the Payer Address.
- Update the Patient Demographics.
- Resubmit the Claim electronically, or print and mail the Claim.
Learn More
Workers Comp and Jopari Electronic Attachments
Related Articles
Workers Comp and Jopari Electronic Attachments
Attach Documents using the Claim Attachments Link This is a Premium Add-On feature. Create a Manage Services Ticket for Jopari setup and activation of this feature. The Electronic Document attachment works independent of a connection to an EHR/EMR, ...Payer Rejections
Payer Rejections Overview Payer Rejections Overview When a Claim is submitted electronically, the information on the individual Claim is matched with the information the Payer has on file. If the information is not in alignment with the Payer ...Rejected Claims on the Encounter by Status Panel
Three Categories of Rejections These Rejections are found in the Encounter by Status Panel on the Claims Management Dashboard or Home Dashboard if pinned. Local Edit Errors (LE) The Local Edit Errors are System delivered rules to catch specific ...Rejections Examples
Rejection: Invalid Subscriber ID Format for ___ Resolution: From the Patient Dashboard, verify Eligibility, view the Eligibility Report, view the Patient's Scanned Insurance Card, and/or call the Patient. Correct the Policy Number. On the Encounter ...Encounters by Status Panel Overview
Access the Encounters by Status panel on the Claims screen or the Home Dashboard if pinned. This panel is used for short-term Claims management. The Filters can be used to search for a specific Insurance, Facility, and Billing Provider and to Include ...