Payer Rejection: INVALID FILING INDICATOR CODE 'CI'
PE: A6 PSBR0905-INVALID FILING INDICATOR CODE 'CI' PSBR0906-INVALID FILING INDICATOR CODE 'CI'
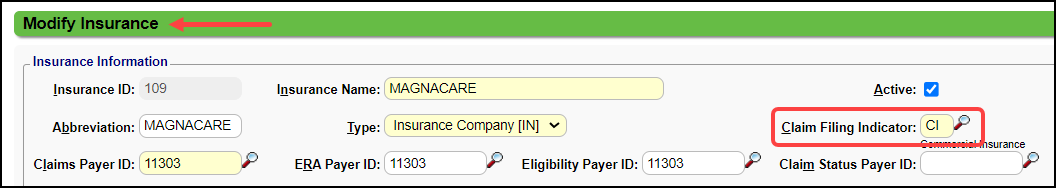
The Claims Filing Indicator (CFI) is not correct.
Resolution: Check the Claims Filing Indicator on the Insurance.
Example: The CFI is CI (Commercial) in the System, but the Payer is BCBS and the CFI should be BL.
Make the change and resubmit the Claim.
Related Articles
Payer Rejections
Payer Rejections Overview Payer Rejections Overview When a Claim is submitted electronically, the information on the individual Claim is matched with the information the Payer has on file. If the information is not in alignment with the Payer ...Payer Rejection Articles
Payer Rejections Payer Rejections Overview Acknowledgement/Receipt Payer Rejection: A6 -A1-;Acknowledgment/Receipt Adjudication Date Payer Rejected: INVALID ADJ PAYMENT DATE Claim Filing Indicator (CFI) Payer Rejection: INVALID FILING INDICATOR CODE ...Rejection: Invalid ZIP code on Subscriber Loop. Bad ZIP 06479 [CE]
CLEARINGHOUSE REJECTED: A7:0 Invalid ZIP code on Subscriber Loop. Bad ZIP 06479 [CE] The Zip Code is invalid for the Subscriber, Loop 2010BA. If Subscriber is the Patient, check the Zip Code in the Patient's Demographics. If Subscriber is not the ...Payer Rejection: Smart Edit
Medicare started the concept of Smart Edits. The Claim rejects at the Clearinghouse level with an alert explaining that the Claim may be denied when processed. Some claims are rejected by a Smart Edit and do not enter the claims processing system. ...Add NDC Numbers (National Drug Code)
The National Drug Code (NDC) serves as the FDA's identifier for drugs. The drugs are identified and reported using a unique, three-segment number applying the 5-4-2 rule. The first segment has 5 digits, the second segment has 4 digits, and the third ...