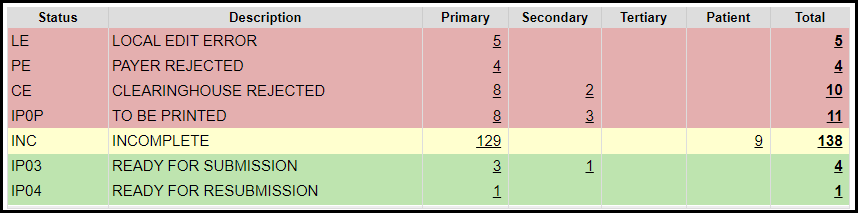
Encounters by Status Panel Overview (Claim Status)
Encounters by Status
Access the Encounters by Status panel on the Claims screen or the Home Dashboard if pinned. This panel is used for short-term Claims management.
The Filters can be used to search for a specific Insurance, Facility, and Billing Provider and to Include Hidden Statuses.
Many times, a Tag can be used instead of a Claim Status. One of the many advantages of Tags is the ability to have more than one Tag on an Encounter. Learn more: Tags.
Claim Statuses
All Encounters when created are assigned a Claim Status.
IP03: Insurance Claims: Ready for Submission
BALANCE: Self Pay Encounters: Assigned Claim Status is Balance
As the Encounters move through the process of submission, the Claim Status changes with each step.
CA: Clearinghouse Accepted CA: Claim passed Clearinghouse edits
EP01: Sent to Clearinghouse: Claim passed the Local Edit errors
EPX: Crossed from Primary: Claims that have been transferred to the Secondary Payer by the Primary Payer.
FP: Finalized Paid
HCOB: Hold Coordination of Benefits: This status is a holding place for the Secondary, Tertiary, and Patient. When the responsible party's payment is posted, this status automatically changes to Ready for Submission for the next Insurance Payer. If the next responsibility is the Patient, the Status changes to Balance.
INC: Incomplete: Claims that have not been completed for submission. Usually, these Claims are created from your Clinical Documentation, but also can be manually marked as Incomplete. These Claims will not be transmitted until they are completed.
PX: Claim Proxied: This status is only available when enrolled in Proxy services.
IPH: On Hold: Manually chosen to keep a claim from being transmitted. Tags can be used for holding claims as well.
IP04: Ready for Resubmission
IP06: Ready for Submission Zero Balance
IP0U: To Be Uploaded Electronically
This is a System Status that is used when Claims that have been batched but are waiting to be uploaded to the Clearinghouse.
This status should NEVER be chosen manually since it is an automatic System function.
Once the Claims are uploaded, the Claims will move automatically to a different status.
IP0P: To Be Printed
NOBAL: No Balance
PA: Payer Accepted: Claim passed Payer edits
PRINT: Has been Printed
SP: Sent to Payer: Claim passed Clearinghouse edits
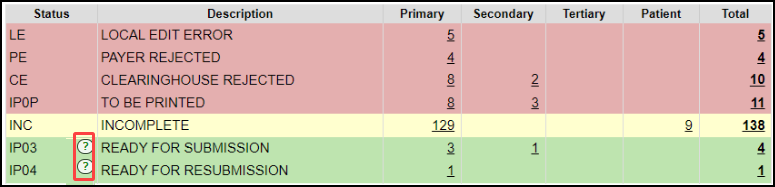
Claim Status Errors
If there are Errors that cause the claim not to transmit, the Encounters by Status panel will show these Statuses:
LE: Local Edit Error: The Claim did not pass the internal System edits.
Charge Management Rules can be used to create additional scrubs before the Claim leaves the System.
These will display on the Encounters by Status panel as Local Edit Errors [LE].
CE: Clearinghouse Rejected: The Clearinghouse provides immediate scrubs to prevent Payer rejections. The rejection reason will indicate how to correct the Claim.
PE: Payer Rejected: Payer Rejections can be more difficult to read as they often do not comply with standard responses.
You may need to contact the Payer directly if you are unsure how to make corrections to resubmit.
***Keep in mind that this Claim has not entered the Payer adjudication system, therefore, it will not be on file at the Insurance Company.***
The Payer should be able to help you with the rejection reason even though they do not have the Claim on file.
Why did my Claims not Batch
If you are confused about why your Claims did not batch, use the Question Marks on the Encounters by Status Panel for further clarification.
The Claims Submission Queue breaks down the reasons down by Category, such as Open Reference Batch, Adjudication Unbalanced, etc.
Learn More
Customize the Encounter by Status Panel
Rejected Claims on the Encounter by Status Panel
Encounter by Status FAQs
Encounter By Status List
Payer Rejections
Charge Management Rules
Related Articles
Rejected Claims on the Encounter by Status Panel
Three Categories of Rejections These Rejections are found in the Encounter by Status Panel on the Claims Management Dashboard or Home Dashboard if pinned. Local Edit Errors (LE) The Local Edit Errors are System delivered rules to catch specific ...Payer Rejection: Reason Not Clear
Payer Rejection: Reason Not Clear Payer Rejection prefixes: EP: Third-Party Clearinghouse AP: Payer Contact the Payer Payer Rejections can be more difficult to read as they often do not comply with standard responses. For Payer rejections that you ...Claim Batch History
The Claim Batch History screen shows a list of all Claim Batches that have been created. Select Claims on the Left Side Menu. In the Claim Submission Queue panel, select the Claim Batch History link. Claim Batch History 1-2 Filter Criteria: Use the ...Send Replacement/Corrected Claim/Delayed Reason/Void
Denial vs Rejection A Denial is a Claim that the Payer has adjudicated but is denying Payment on one or more Charges on the Claim. You have either received a Paper or Electronic Remittance with the denial. Denied Charges can be resubmitted as a ...Real-Time Claim Status
*This is a Premium Add-on feature. Common Problems with manually checking Claim Status Challenge of timely follow-up on Insurance Claims that are delayed or have no response from the Payer. A Claim can appear to be Payer Accepted, but the Claim has ...