Rejection: Adjudication Date (2430*DTP*573) Cannot be Earlier than Service Date
Reason for Rejection
This occurs when you have posted a primary payment and are sending the claim to a secondary payer. When posting the payment, you were attached to a Reference batch whose Post Date is before the Date of Service. Usually, this is accidental because you were in another batch and forgot to attach to a current Reference Batch. It is always best to make sure you are attached to a current batch when posting.
To fix this rejection if the Receipt and Posted Payment are in the same batch:
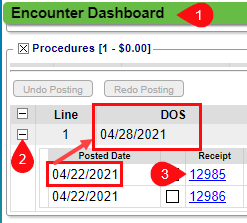
Go to the Encounter Dashboard.
Expand the line Items on the Encounter to find the Receipt with the incorrect post date.
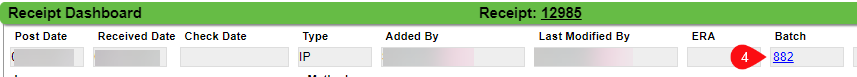
Click the Receipt number to go to the Receipt Dashboard. (Make note of the receipt number.)
On the Receipt Dashboard, click the Reference Batch Number.
Enter the Receipt number in the Filter.
Click Search.
Select the box next to the Receipt number.
Click Change Batch.
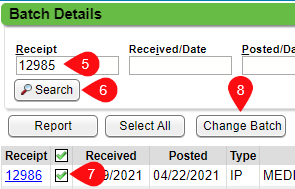
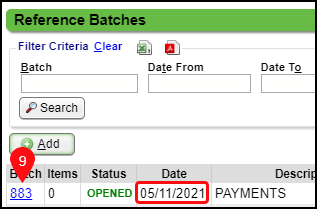
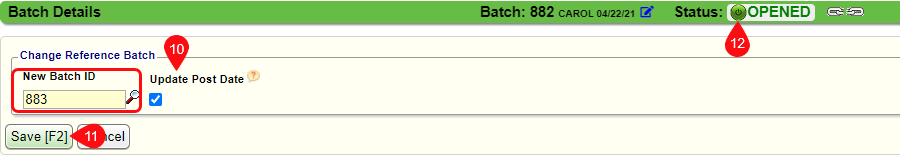
Choose a Reference Batch that has a Post Date later than the Date of Service. (Both Reference Batches must be Open.)
Check the box for Update Post Date.
Click Save [F2].
Click the green circle to close the Reference Batch.
If the Receipt was entered in the correct Reference Batch, but the payment was not posted using that same Batch
The receipt was entered in one Reference Batch, but the user was connected to a different Reference Batch when it was posted to the Encounter. The receipt and the posted payment must be connected before it can be moved. You cannot move a posted payment by itself because it does not show in the Reference Batch as an item.
Learn More
Related Articles
Clearinghouse Rejection Articles
If the Subscriber State (AB) is a Canadian province then Subscriber Zip Code (AB T8L0S2) must be six characters Referring Provider (23010A) is required to be a person 2300 NTE02 has a character limit of 80 characters Service Line 1 COB Claim ...Clearinghouse Rejection: Service Line 1 COB Claim adjudication date
CE: Service Line 1 COB Claim, adjudication date is required for payer id 'MCRTX' Service Line 1 COB not balanced; Line Payments + Line Adjustments do not equal Line Billed Amount for Payer id MCRTX (Loop 2430) ***MCRTX is being used in the example. ...Payer Rejection Articles
Payer Rejections Payer Rejections Overview Acknowledgement/Receipt Payer Rejection: A6 -A1-;Acknowledgment/Receipt Adjudication Date Payer Rejected: INVALID ADJ PAYMENT DATE Claim Filing Indicator (CFI) Payer Rejection: INVALID FILING INDICATOR CODE ...Payer Rejections
Payer Rejections Overview Payer Rejections Overview When a Claim is submitted electronically, the information on the individual Claim is matched with the information the Payer has on file. If the information is not in alignment with the Payer ...Rejections Examples
Rejection: Invalid Subscriber ID Format for ___ Resolution: From the Patient Dashboard, verify Eligibility, view the Eligibility Report, view the Patient's Scanned Insurance Card, and/or call the Patient. Correct the Policy Number. On the Encounter ...