Real-Time Claim Status
*This is a Premium Add-on feature.
Common Problems with manually checking Claim Status
Challenge of timely follow-up on Insurance Claims that are delayed or have no response from the Payer.
A Claim can appear to be Payer Accepted, but the Claim has not yet been adjudicated.
If the Payer is contacted, the Claim will not be on file until it is adjudicated.
The manual process for checking a Claim's status is extremely time-consuming, costing valuable User productivity for your practice.
Long hold times
Navigating IVR systems
Inquiries on many different Payer portals that have short password expirations.
Lock outs for bad login attempts.
The result is lost revenue.
Advantages of using Real-Time Claim Status
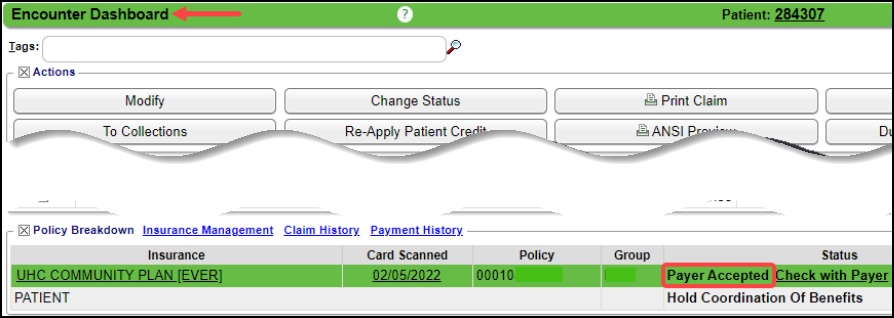
- Real-Time Claim Status (RTCS) is an electronic method of getting an immediate Claim Status update from the Payer. If the Claim shows a Status of Payer Accepted on the Encounter Dashboard and the Payer offers RTCS, the option Check with Payer link will be available for checking Real-Time Claim Status. (Encounter Dashboard > Policy Breakdown panel > Insurance line > Check with Payer)
- Since the Claim has reached adjudication, there will be no wasted User time contacting the Payer before adjudication.
- The Last Checked Date makes it easy to view the last Claim Status results and should also help prevent unnecessary Real-Time Claim Status checks.
- When RTCS is used, the exact same information that was sent in Claim Loop 2010AA will automatically be sent on the Claim Status Request.
- This is EIN/SSN and NPI of the entity to whom the Insurance Payment is directed.
- It ensures proper matching and response from the Payer.
- This information is required whether checking Claim Status using RTCS or manually checking.
- Real-Time Claim Status can be configured to run automatically using the Job Scheduler, eliminating the need for User intervention.
Payers with Real-Time Claim Status
On the Enrollment screen and the Clearinghouse Payer List, you can view a list of Payers that offer Real-Time Claim Status.
- Home Dashboard > Enrollments button
- To see the ones that need Enrollments to be completed, select Only for Enrollment Required (scroll to the right). Select Search.
- To see all of the Payers that offer Real-Time Claim Status, select Include for Enrollment Required. Select Search.
- The Action column will display whether the Payer requires Enrollment.
- Admin > Clearinghouse Payer List button
- Select Claims Status for Type.
- This will produce a list of all Payers with Real-Time Claim Status along with Payer ID and the State designation if applicable.
- To see only the ones that need Enrollments, select Claim Status for Type, and Yes for Enrollment Required. Select Search.
- To see Enrollments for your State only, select Claim Status for Type, Yes for Enrollment Required, and select your State in the State filter. Select Search.
- Enrollments must be done from the Enrollments button on the Home Dashboard.
Learn More
Related Articles
Real-Time Eligibility Responses/Errors
These are responses that you may receive when doing an Eligibility Check. While some responses may indicate a Payer issue. Mostly, these indicate a problem with the Insured/Policy Holder Name, address, Policy Number, or Medicare Advantage Plans. ...Automate Real-Time Claim Status with the Job Scheduler
*Real Time Claim Status is a Premium Add-On Feature. Real-Time Claim Status (RTCS) allows the System to automatically check Claim Status responses on a designated schedule. This helps keep Claim Statuses up-to-date without requiring manual follow-up ...Premium Add-On Features
If you are interested in the Premium add-on features, create a Manage Services ticket. Following the instructions using this link: MS Manage Services. Balance Notifications Provides scheduled Patient balance notifications. Credit Card Services ...Interactive Aging: Real-Time A/R View
Interactive Aging: Real-Time A/R View This report is not meant to balance to the Period End Report. The Interactive Aging Report is a real-time A/R Report. It can be grouped and aged dynamically. If the Bill Date is chosen as the Aging Date, and ...Customize the Encounter by Status Panel (Claim Status)
The Encounter by Status Panel can be customized by moving and/or adding Claim Statuses. Change the Order of the Claim Statuses On the Libraries screen, select the Claim Status button. Change the order the Statuses appear in the Encounters by Status ...