Payer Rejections
Payer Rejections Overview
When a Claim is submitted electronically, the information on the individual Claim is matched with the information the Payer has on file.
If the information is not in alignment with the Payer Information, the Claim is rejected and not accepted for adjudication.
Do not confuse this with a Payer Denial, which is totally different.
 A Payer Rejection is not the same as a Payer Denial. A rejection gets kicked back before it enters the Payer's system. A Denial has been adjudicated, and Payment has been denied.
A Payer Rejection is not the same as a Payer Denial. A rejection gets kicked back before it enters the Payer's system. A Denial has been adjudicated, and Payment has been denied.Payer Rejected Claims are not adjudicated and, therefore, are not in the Payer's System.
If you call the Payer on this Claim, it will not be found in their system.
The Payer should be able to tell you what the rejection message means in general.
Check the Information on the Insurance Card.
Member ID
Policy Holder
Check the Payer ID
Patient Information
Date of Birth (DOB) is a common reason for rejection.
The Insured's or Patient's Name is not the same as the Insurance Information.
Patient address
Diagnosis/Procedure Codes
Invalid/Inactive Procedure Code
Invalid/Inactive Diagnosis Code
Modifier is incorrect or required.
Taxonomy
Incorrect Taxonomy Code
TIN or NPI is not on file with the Payer.
Learn More
Denial Worklist Overview
Add a Manually Posted Insurance Denial to a Worklist
Acknowledgement/Receipt
This does not mean that the claim has been accepted for adjudication.;Entity acknowledges receipt of claim/encounter.;Payer-A7-;Rejected for Invalid Information;HCPCS;S9999-Reference line item control number 12354E123456L2; Procedure Code S9999; Total Charges 7.14
Resolution for resubmission:
Exclude the Line Item with the invalid HCPCS.
Change it to a valid Procedure Code.
Claim Filing Indicator (CFI)
The Claims Filing Indicator (CFI) is not correct.
Resolution: Check the Claims Filing Indicator on the Insurance.
Example: The CFI is CI (Commercial) in the System, but the Payer is BCBS and the CFI should be BL.
Make the change and resubmit the Claim.
Claim Frequency Code
PE: A6 Rejected for Invalid Information; Claim Frequency Code
The Payer does not accept "Replacement" as the Frequency Code (usually Medicare).
Resolution: Change the Frequency from Replacement to Original on the Modify Charge screen. (Encounter Dashboard > Modify button > Claim (found at bottom of screen) > Original)
CLIA (Clinical Laboratory Improvement Amendment)
PE: A6 A7-0- Rejected for Invalid Information - Cannot provide further status electronically
A7-544- Rejected for Invalid Information - Clinical Laboratory Improvement Amendment
Rejected for CLIA number.
Resolution: Enter the CLIA number on the Service Facility.
Dates of Service
ERROR NO MEMBER ID MATCH FOR 'TEST,BOBBY H12345678' BY SERVICE DATE NOT ELIGIBLE
The Subscriber was not found or was not eligible on the DOS.
Resolution:
Compare the Insurance Card on file with the information in the System.
Is the Claim being sent to the correct Payer?
Verify who the Policy Holder is.
Check Eligibility.
Verify with Patient.
Detailed Description for Service
Resolution: The Encounter needs a description entered in the note field on the line item.
Go to the Encounter Dashboard.
Choose the Modify button.
Select the Line item of the CPT® that was rejected.
In the Note field, enter a more detailed description for the Procedure.
Select Save [F2].
Select Save [F2] again.
Entity not Affiliated
A6 -A7-;Rejected for Invalid Information;Entity not affiliated. Usage- This code requires use of an Entity Code.;
Reason for Rejection
Enrollment may need to be completed for Claims to be sent to this Payer.
Resolution
Verify that enrollment has been done for this Payer and/or you have chosen the correct Payer.
Entity not Eligible
ERROR NO MEMBER ID MATCH FOR 'TEST,BOBBY H12345678' BY SERVICE DATE NOT ELIGIBLE
The Subscriber was not found or was not eligible on the DOS.
Resolution:
Compare the Insurance Card on file with the information in the System.
Is the Claim being sent to the correct Payer?
Verify who the Policy Holder is.
Check Eligibility.
Verify with Patient.
Entity not Found: Patient/Insured/Subscriber/Dependent
- The Patient is no longer covered by this Insurance Plan.
- Resolution: Get new Insurance Information from the Patient.
- The Claim was sent to the wrong Payer.
- Resolution: Check Insurance Information to validate the Payer and Payer ID. Make corrections if necessary.
- Invalid/Missing/Incorrect Insured information.
- Submitted incorrect information:
- Name of Insured/Subscriber could be spelled incorrectly.
- The name on the Insurance card may not be the name you have in the System.
- The birthdate could be incorrect.
- Resolution: Correct if necessary.
- Invalid/Missing/Incorrect client/Patient information.
- Misspelled Name
- Wrong Birthdate
- Resolution: Make corrections.
Facility NPI Loop 2310D
PE: A6 -A3-;Rejected;Missing or invalid information.
Note- At least one other status code is required to identify the missing or invalid information.;-ELEMENT NM109 IS USED. IT IS NOT EXPECTED TO BE USED WHEN IT HAS THE SAME VALUE AS ELEMENT NM109 IN LOOP 2010AA. SEGMENT NM1 IS DEFINED IN THE GUIDELINE AT POSITION 2500. INVALID DATA 1811070790-; [PE]
The Payer does not want the NPI in the Facility loop if it is the same as the Billing.
Resolution: Add following Insurance ID to the Insurance to remove NPI in the 2310D, Facility.
Payer specific
Type: FNPI (You may have to add it to the lookup)
ID: Enter the actual word, BLANK
HCPCS S9999
PE: A6 -A1-;Acknowledgement/Receipt-The claim/encounter has been received.
This does not mean that the claim has been accepted for adjudication.;Entity acknowledges receipt of claim/encounter.;Payer-A7-;Rejected for Invalid Information;HCPCS;S9999-Reference line item control number 12354E123456L2; Procedure Code S9999; Total Charges 7.14
Resolution for resubmission:
Exclude the Line Item with the invalid HCPCS.
Change it to a valid Procedure Code.
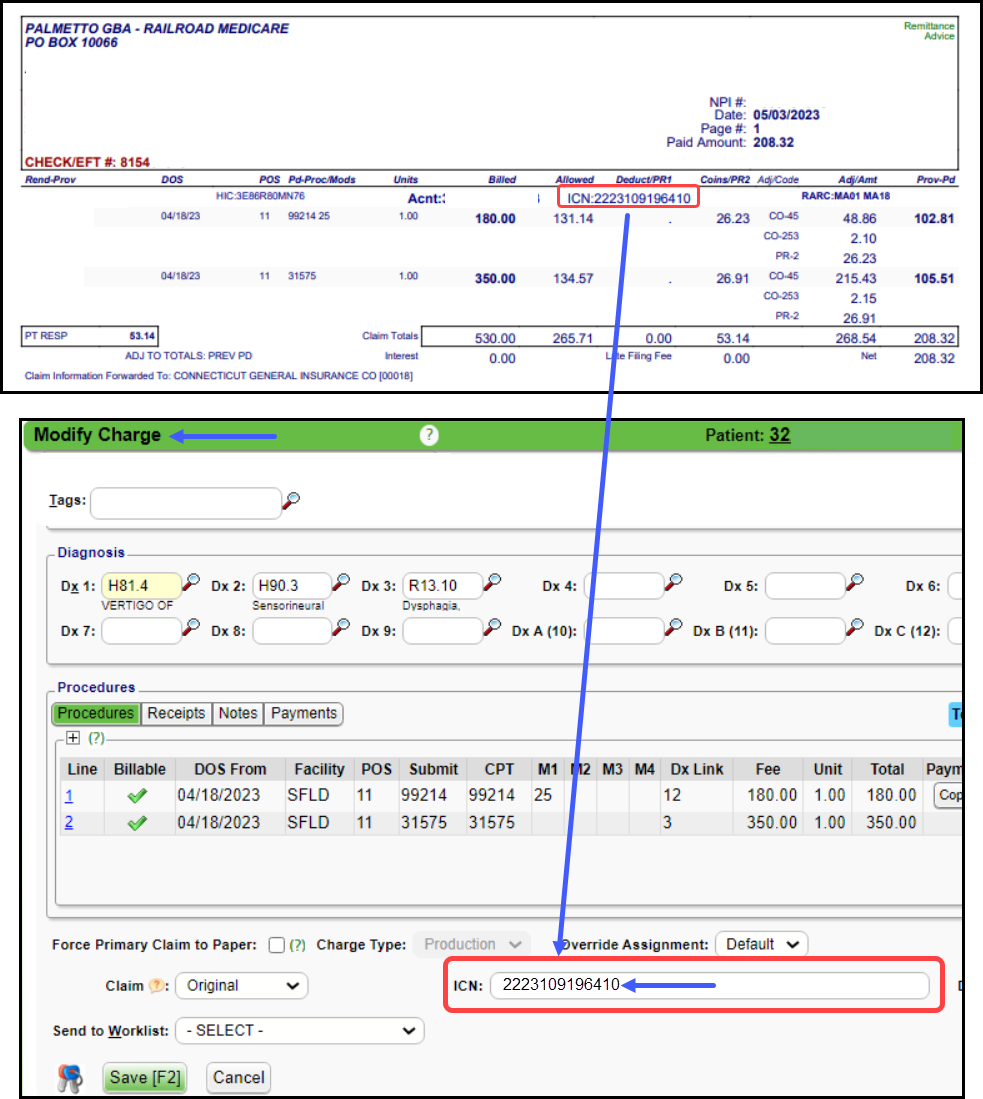
ICN (Internal Control Number)
- The ICN Number is missing for a previously adjusted claim.
- Resolution: Find the ICN number on the Remit and add it to the Claim.
Invalid Adjustment Payment Date
PE A6 GB; PDT0303 INVALID ADJ PAYMENT DATE
Rejected; Other Entity's Adjudication or Payment/Remittance Date. Note- An Entity code is required to identify the Other Payer Entity i.e. primary secondary.;Payer
If the Claim has been crossed by Medicare, it will be paid regardless of Paid Date from the Primary. (Mainly a BCBS issue)
IF the claim is manually sent to the Secondary Payer, and it is under 30 days from the Primary Adjudication Date, the secondary Payer will reject the Claim.
Invalid Information: Another Insurance
Processed according to plan provisions (Plan refers to provisions that exist between the Health Plan and the Consumer or Patient)
If this is from Medicaid, it usually means the Payer thinks there is different insurance.
Resolution: Verify the Insurance.
Invalid Information: File with Medicare as Primary
A7-284- Rejected for Invalid Information - Copy of Medicare ID card. -
Invalid Information: Claim Frequency Code
The Payer does not accept "Replacement" as the Frequency Code (usually Medicare).
- Resolution: Change the Frequency from Replacement to Original on the Modify Charge screen.
- Encounter Dashboard > Modify button > Claim dropdown (found at bottom of screen) > Original
- Learn More: Replacement Claim/Auto-Populate with Corrected Claim
Invalid Information for Member Number
PAYER REJECTED
A6-A7-;Rejected for Invalid Information;Entity's contract/member number.;Insured or Subscriber-A7-;Rejected for Invalid Information;Entity not eligible for benefits for submitted dates of service.;Insured or Subscriber [PE]
A6 -A3-;Rejected;Missing or invalid information. Usage- At least one other status code is required to identify the missing or invalid information.;-PAYER SECONDARY IDENTIFIER INVALID; MUST BE A VALID CLAIM OFFICE NUMBER FOR PAYER-;-A3- ;Rejected;Missing or invalid information. Usage- At least one other status code is required to identify the missing or invalid information.;-DESTINATION PAYER PRIMARY IDENTIFIER INVALID; MUST BE A VALID PAYER ID FROM THE EMDEON PAYER LIST-;
A6 -A1-;Acknowledgement/Receipt-The claim/encounter has been received. This does not mean that the claim has been accepted for adjudication.;Claim Note Text;-PAYER ACKNOWLEDGED RECEIPT OF THE CLAIM-;-A1-;Acknowledgement/Receipt-The claim/encounter has been received. This does not mean that the claim has been accepted for adjudication.;Entity acknowledges receipt of claim/encounter.;Receiver-A3-;Rejected;Returned to Entity.;Payer-A1-;Acknowledgement/Receipt-The claim/encounter has been received. This does not mean that the claim has been accepted for adjudication.;Claim Note Text;- ACKNOWLEDGEMENT/RECEIPT-THE CLAIM/ENCOUNTER HAS BEEN RECEIVED. THIS DOES NOT MEAN THAT THE CLAIM HAS BEEN ACCEPTED FOR ADJUDICATION.ENTITY ACKNOWLEDGES RECEIPT OF CLAIM/ENCOUNTER.-;-A3- ;Rejected;Claim Note Text;-R VALID REFERRAL FORMAT REQUIRED-;
A6 -A7-;Rejected for Invalid Information;Entity's National Provider Identifier (NPI).;Rendering Provider
A6 ACK/RETURNED - REQUESTS FOR RE-ADJUDICATION MUST REFERENCE THE NEWLY ASSIGNED PAYER CLAIM CONTROL NUMBER FOR THIS PREVIOUSLY ADJUSTED CLAIM. CORRECT THE PAYER CLAIM CONTROL NUMBER AND RE-SUBMIT
A6 ACK/REJECT INVAL INFO - ENTITYS NATIONAL PROVIDER IDENTIFIER (NPI). USAGE- THIS CODE REQUIRES USE OF AN ENTITY CODE. - REFERRING PROVIDER | 99214 SVC02=180 FJ02=517853E353573L1 Data- SVC01=HC
A6 ACK/REJECT INVAL INFO - ENTITYS NATIONAL PROVIDER IDENTIFIER (NPI). USAGE- THIS CODE REQUIRES USE OF AN ENTITY CODE. - REFERRING PROVIDER | 99204\ Data- SVC01=HC\ | 31231 SVC02=365 FJ02=517853E350198L2 DataSVC01=HC\ | 30903\ Data- SVC01=HC
A6 99204\ Data- SVC01=HC\ | 30903\ Data- SVC01=HC\ | 31231 SVC02=365 FJ02=517853E350198L2 Data- SVC01=HC\ | ACK/REJECT INVAL INFO - ENTITYS NATIONAL PROVIDER IDENTIFIER (NPI). USAGE- THIS CODE REQUIRES USE OF AN ENTITY CODE. - REFERRING PROVIDER
A6 -A3-;Rejected;Missing or invalid information. Usage- At least one other status code is required to identify the missing or invalid information.;-ACK,RETURND AS UNPRCESSBLE CLM- CLM,ENCNTER BEEN REJECTD AND NOT ENTERD INTO ADJUDICATION SYS. MISSING OR INVALID INFORMATION-
A6 -A7-;Rejected for Invalid Information;Missing/invalid data prevents payer from processing claim. (Use CSC Code 21);- ACKNOWLEDGEMENT RECEIPT-THE CLAIM ENCOUNTER HAS BEEN RECEIVED. THIS DOES NOT MEAN THAT THE CLAIM HAS BEEN ACCEPTED FOR ADJUDICATION. RECEIVER ACCEPTED FOR PROCESSING.-;-A7-;Rejected for Invalid Information;Missing/invalid data prevents payer from processing claim. (Use CSC Code 21);-ACKNOWLEDGEMENT RECEIPTTHE CLAIM ENCOUNTER HAS BEEN RECEIVED. THIS DOES NOT MEAN THAT THE CLAIM HAS BEEN ACCEPTED FOR ADJUDICATION. PAYER ACKNOWLEDGES RECEIPT OF CLAIM ENCOUNTER.-;-A7-;Rejected for Invalid Information;Missing/invalid data prevents payer from processing claim. (Use CSC Code 21);-ACKNOWLEDGEMENT RETURNED AS UNPROCESSABLE CLAIM-THE CLAIM ENCOUNTER HAS BEEN REJECTED AND HAS NOT BEEN ENTERED INTO THE ADJUDICATION SYSTEM. SUBSCRIBER PATIENT ELIGIBILITY NOT FOUND WITH ENTITY.-;-A7-;Rejected for Invalid Information;Missing/invalid data prevents payer from processing claim. (Use CSC Code 21);-R REJECTED-;
A6 ACK/RETURNED - ENTITY NOT ELIGIBLE FOR MEDICAL BENEFITS FOR SUBMITTED DATES OF SERVICE. USAGE- THIS CODE REQUIRES USE OF AN ENTITY CODE
A6 ACK/REJECT INVAL INFO - ENTITYS NATIONAL PROVIDER IDENTIFIER (NPI). USAGE- THIS CODE REQUIRES USE OF AN ENTITY CODE. - REFERRING PROVIDER
A6 ACK/RETURNED - ENTITY NOT ELIGIBLE FOR MEDICAL BENEFITS FOR SUBMITTED DATES OF SERVICE. USAGE- THIS CODE REQUIRES USE OF AN ENTITY CODE.
A6 -A3-;Rejected;Cannot provide further status electronically.;Payer-02 - INVALID MBR-;
A6 -A3-;Rejected;Cannot provide further status electronically.;Payer-09 - MBR NOT VALID AT DOS
A6 ACK/RETURNED - REQUESTS FOR RE-ADJUDICATION MUST REFERENCE THE NEWLY ASSIGNED PAYER CLAIM CONTROL NUMBER FOR THIS PREVIOUSLY ADJUSTED CLAIM. CORRECT THE PAYER CLAIM CONTROL NUMBER AND RE-SUBMIT.
A6 SUBSCRIBER PRIMARY IDENTIFIER- INVALID; MUST NOT BE EQUAL TO 0'S, 1'S, 2'S, 3'S, 4'S, 5'S, 6'S, 7'S, 8'S, 9'S OR THE LITERALS INDIVIDUAL, 1234567890, 123456789, UNKNOWN, SELF, OR NONE AND MUST BE A MINIMUM OF TWO CHARACTERS IN LENGTH
A6 ACK/RETURNED - CLAIM SUBMITTED TO INCORRECT PAYER
A6 -A3-;Rejected;Entity's contract/member number.;
A6 Etactics Note- Claim has previously rejected on earlier report; New Message(s) - -A2-;Acceptance into adjudication system;Accepted for processing
A6 -P5-;Pending/Payer Administrative/System hold;Verifying premium payment;
Invalid Information: File with Medicare as Primary
A7-284- Rejected for Invalid Information - Copy of Medicare ID card. -
Length Invalid
Note: At least one other status code is required to identify the data element in error.;-A7-;Rejected for Invalid Information;Submitted charges
Reason for rejection:
The payer cannot process the claim amount over $100,000,000.
To fix this this rejection:
Correct the fee amount, and resubmit the claim to the payer.
Member ID Mismatch on Date of Birth
- The member ID and Date of Birth do not match.
- Resolution: Correct DOB.
MSP Code for Medicare Secondary Claims
Payer Rejected
Rejection: Element SBR05 Must Contain ___ , or Claims with Medicare as Secondary Payer Require Valid MSP Type Code
OR
Clearinghouse Rejected
A7:0
For Medicare Secondary Claims, the Secondary Insurance Type Code must be one of the following 12,13,14,15,16,41,42,43, or 47. Insurance Type Code Mandatory for MSP claims Element
This indicates that Medicare is not the Primary payer.
A special code defining the Primary Insurance's nature (like group health, auto, or disability) is required in segment SBR-05 (Loop 2000B)
Resolution
From the Patient or Encounter Dashboard, go to the Patient's Insurance Policy.
In the Policy Breakdown panel on the Encounter or Patient Dashbaord, select Medicare that is in the secondary position.
In the Medicare Secondary Reason dropdown list, choose the reason Medicare is the Secondary Payer (MSP).
The lookup contains all valid MSP reason codes.
If you check eligibility, the reason is stated in the Eligibility Report.
Select Save [F2].
On the Encounter Dashboard, change the Claim Status to Ready for Submission/Resubmission.
NDC
Rejection for NDC
- Reason for rejection
- The NDC is incorrect. The Clearinghouse drops the hyphens (dashes).
- Resolution
- Update the J code with the correct NDC and resubmit.
Not Eligible Payer Rejected
The Claims with this Payer Rejection did not make it into the Payer adjudication system. If you call the Payer, they will not have a record of this Claim.
Options
- Call the Patient for updated Insurance information or
- Go to the Encounter Dashboard and move the Encounter to Self Pay to create a Statement when Statements are run.
- For an ERA, post the $0.00 payment and drop the responsibility to the Patient.
- If you do not want to write off the balance, do not post the CO codes because that will drop the balance to zero, and the Patient will not get billed.
Move the Encounter to Self Pay
- If there are Transactions posted that are not Patient Payments or Copays, the Encounter cannot be moved to Self Pay.
- If there are no Transactions or the only Transaction Codes on the Encounter are PP, PIPPR, Or PIPPB, the Encounter can be moved to Self Pay.
Steps to Move the Encounter to Another Insurance
- Select Insurance Management on the Encounter Dashboard.
- Highlight the Insurance Profile where the Encounter is located.
- At the bottom of the screen, select the check box beside the Encounter number.
- Select the Change Profile/Rebill button.
- To New Profile: Select Self Pay from the dropdown menu.
- Update Fees: If there is a different Fee Schedule for Self Pay, leave the checkbox selected if you want the fee to change.
- Uncheck if the fee should not change.
- Transfer Balance From Patient To: Defaults to Leave Balance with Patient
- Uncheck the Re-Bill checkbox.
- Claim History Note: Enter a Note if applicable.
- Save as Billing Note: Select the checkbox if the note should be saved as a Billing Note.
- Select Save [F2].
NPI
Rejection for NPI
R^^Category- Acknowledgement/Rejected for Invalid Information - The claim/encounter has invalid information as specified in the Status details and has been rejected. Status- Entity's National Provider Identifier (NPI)^^^ [PE]
Reason for rejection
NPI does not match the Payer's records.
Resolution
Verify the NPI with the Payer.
NUBC Occurrence Code
PE: NUBC OCCURRENCE CODE- check the Revenue code - an occurrence code is required
An Occurrence Code is required for ER Revenue Code.
An ER revenue code must have an occurrence code of '01' OR '02' OR '03' OR '04' OR '05' OR '06' OR '11'
Example: occurrence code 11 Onset date of symptom or illness.
Other Insurance Coverage
A6 ACK/REJECT MISS INFO - OTHER INSURANCE COVERAGE INFORMATION (HEALTH, LIABILITY, AUTO, ETC.).
PE A7-104- Rejected for Invalid Information.
Processed according to plan provisions (Plan refers to provisions that exist between the Health Plan and the Consumer or Patient)
If this is from Medicaid, it usually means the Payer thinks there is different insurance.
Resolution: Verify the Insurance.
Previously Rejected
Reason for rejection
The Claim was sent to the Payer and was rejected.
The claim was resubmitted to the payer without making the changes.
Resolution
On the Encounter Dashboard, select the Claim History link in the Policy Breakdown panel.
In the Filter Criteria, select Payer Rejected from the Status dropdown list.
Review the earlier rejection to identify the required changes.
In the following figure, the NDC needs to be corrected.
Procedure Code - Non Specific
PE SUB-ELEMENT SV101-07 IS MISSING.
IT IS REQUIRED WHEN PROCEDURE CODE IS NON-SPECIFIC (SV101-02 IS J3301). SEGMENT SV1 IS DEFINED IN THE GUIDELINE AT POSITION 3.
The non-specific Procedure Code needs a more detailed description.
Resolution: Add a detailed description in the Note Field on the line item.
According to EDI, they move the info to the correct place
NOC (Not Otherwise Classified) codes need a description by Medicare standards.
Some Medicare replacements also require this.
This is sent in 2400 Loop.
Learn More: List of NOC Codes that Require a Description
Procedure Code/Modifiers
Purchase Service Missing
PAYER REJECTED: Missing 2420B Loop; Requires Purchase Service Provider Name and NPI
A6-A3-; Rejected; Missing or invalid information. Usage- At least one other status code is required to identify the missing or invalid information.; -THE PROCEDURE CODE 80061 (2400 SV101-2) SUBMITTED WITH A MODIFIER OP REQUIRES THE PURCHASE SERVICE PROVIDER NAME TO BE SUBMITTED AND THE NPI.-; [PE]
Rejected for: Missing 2420B Loop
Resolution: Outside Lab: If selected, new fields appear for Purchased Service Cost and Laboratory. This data output is required on both paper and electronic Claims. The Billing Provider NPI will output in the ANSI 2420B loop, if the amount in the Purchased Service Cost field is greater than 0.00.
Learn More
Purchased Services
Re-adjudicated Payer Claim Control Number (ICN)
- The ICN Number is missing for a previously adjusted claim.
- Resolution: Find the ICN number on the Remit and add it to the Claim.
Reason Not Clear Payer Rejection
Payer Rejection prefixes
- EP: Third-Party Clearinghouse
- AP: Payer
Contact the Payer
- For Payer rejections that you cannot understand, you will need to contact the Payer directly if you are unsure how to make the corrections to resubmit the Claim.
- Keep in mind that this Claim has not entered the Payer adjudication system, therefore:
- They will not be able to see the Claim, and
- You will not have an EOB.
- Ask for the EDI Department for non-adjudicated claims.
- Even though the Claim has not entered the adjudication system, the Payer should be able to clarify the meaning of the rejection.
- Have this information available:
- Patient's name and date of birth
- Policy Holder's name and date of birth if different than Patient.
- Policy and Group Number.
- Insurance Card should be loaded into the Patient Dashboard and/or the Ticket.
- Payer Rejection Reason that was sent back into the System.
- If the Representative can answer the question, ask for the ANSI Loops and Segments the information needs to be in.
- Ask the Representative if the Policy Number is the correct one to use.
- If the Representative does not give you a clear answer, ask for another Representative.
- Ask if the Payer has a website where the information can be found.
- If they do, get the website address.
- Ask for the name of the person you are speaking with.
- Get a Reference number for the call.
- Document the conversation in the Notes panel of the Encounter/Patient Dashboard and/or on the Worklist item.
- Phone number that was called
- Who did you speak with?
- What is the Reference # of the call?
Options
- If the Payer accepts paper Claims, the HCFA can be mailed to the Payer.
- You may be able to file the Claim on the Payer's Web Portal.
Referral/Authorization Number Rejection
VA COMMUNI [VACCN] PAYER REJECTED
A6 -A3-;Rejected;Returned to Entity.;Payer-R VALID REFERRAL FORMAT REQUIRED-; [PE]
The Claim needs a Referral/Authorization Number.
- The Referral always comes with an Authorization number that starts with VA.
- The Claims will not be processed without this VA number.
- Add a Charge Management Rule to prevent these Claims from being submitted without the Authorization/Referral Number.
Sequestration Missing
Missing Sequestration Adjustment CO253.
Acknowledgement/Rejected for Missing Information. The Claim/Encounter is missing information specified in the Status details and has been rejected Status: Federal sequestration adjustment (CO253).
Rejected for: The Sequestration adjustment is missing.
Resolution: Post the Sequestration Adjustment CO253.
Payer Rejection: Acknowledgement/Rejected for Missing Information. The Claim Encounter is missing Information specified in the Status details and has been rejected Status: Federal Sequestration Adjustment
Medicare will provide the needed adjudication information when they submit a crossover claim to the payer on your behalf. You are receiving this rejection because the claim is missing a Federal Sequestration Adjustment amount (CO253) from Medicare’s claim consideration (835).
Note: Medicare applies a 2% sequestration reduction adjustment to all Claim benefit payments.
- When electronically submitting a secondary (COB) claim on which Medicare has made a payment, the Federal sequestration adjustment amount must be populated from the Medicare remittance using remark/reason code 253, in addition to all other Medicare payment and adjustment amounts.
Sequence Number
Reason for rejection
This Payer does not accept Secondary Claims.
Resolution:
Select the Insurance ID for the Payer.
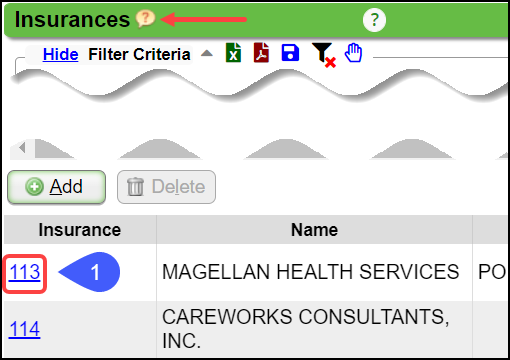
Click Edit.
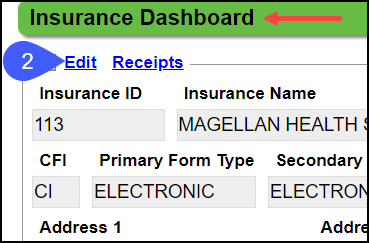
From the Secondary Form Type dropdown list, select HCFA.
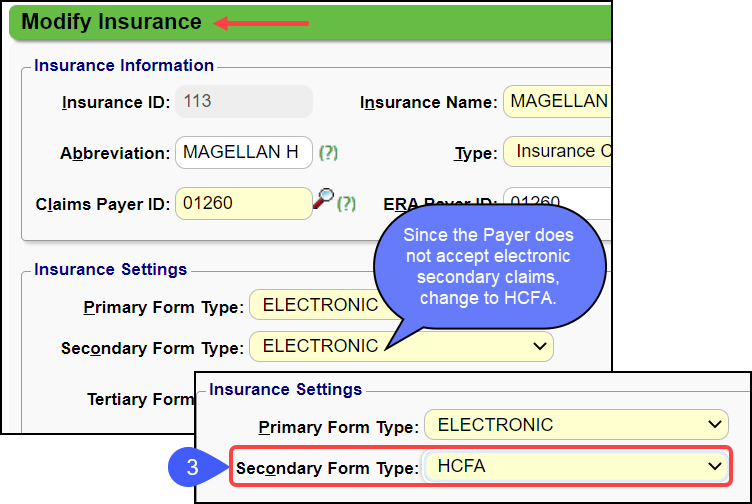
Enter the Payer's Address if not already completed.
Select Save [F2].
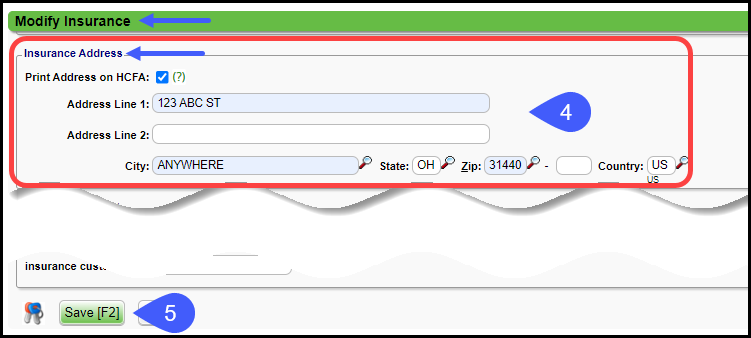
Change the Claim Status to Ready for Submission/Resubmission.
When the Claims are batched, this Claim will drop to paper.
The Claim & Primary EOB can also be printed from the Encounter Dashboard.
Mail the Claim.
Service Date Invalid
This Rejection is for DOS and may be due to:
An incorrect Payer ID.
Patient was not eligible on the DOS.
Patient no longer has this Insurance.
Smart Edit
Medicare started the concept of Smart Edits. The Claim rejects at the Clearinghouse level with an alert explaining that the Claim may be denied when processed.
Some claims are rejected by a Smart Edit and do not enter the claims processing system. These claims must be corrected and resubmitted.
To be processed by Medicare, the claim must be resubmitted.
Other Smart Edits are informational only and will still be passed to the claims processing system for payment consideration.
The following link directs you to Palmetto GBA Advance Clinical Editing (P-ACE) Smart Edits
277CA Edit Lookup Tool (External link)
If you want to send the Claim without making any changes disregarding the Smart Edit warning, change the Claim Status to Ready for Submission/Resubmission.
The Claim response will now be Payer Accepted.
It will be adjudicated by the Payer and visible on the Payer portal.
UHC also utilizes Smart Edits, but their behavior is different from Medicare and likely more common.
If no Claim is resubmitted with changes, UHC will release the Claim for processing after 5 days.
If no changes need to be made, no additional Claim is required
If you want to make changes to the Claim based on the advice of the SmartEdit, make the changes, and send a new Claim which may be subject to a different Smart Edit.
Use these links for more information on UHC Smart Edits: UHC Smart Edits Guide and Smart Edits Lookup (external links).
UHC Smart Edit Example
-A7-;Rejected for Invalid Information;Missing or invalid information. Usage- At least one other status code is required to identify the missing or invalid information.;-P4999REJINFO SMARTEDIT (REJINFO) [PATTERN 53845] INFORMATIONAL - THIS CLAIM HAS BEEN REJECTED AND WILL NOT BE PROCESSED. SEE UHCPROVIDER.COM/SMARTEDITS. REPAIRED CLAIMS SHOULD BE SENT WITH THE ORIGINAL FREQUENCY CODE, NOT A REPLACEMENT OR VOIDED INDICATOR-;-A7-;Rejected for Invalid Information;Missing or invalid information. Usage- At least one other status code is required to identify the missing or invalid information.;-P4999LBI SMARTEDIT (LBI) REJECT - PER LCD OR NCD GUIDELINES, PROCEDURE CODE 99406 HAS NOT MET THE ASSOCIATED DIAGNOSIS CODE RELATIONSHIP CRITERIA FOR CMS ID(S) 210.4.1.-;-Payer Claim Control Number - FLN 940252306498700 ICN FF83454140-; [PE]
The green highlighted items represent the Smart Edit Code that can be used in the lookup on UHC's Smart Edit page: Smart Edits Lookup
The yellow highlighted items provide the status of the Claim and a reason why the Claim was rejected.
Learn More
Resubmit Claims
Status Code
PAYER REJECTED: A6 -A3-;Rejected; Missing or invalid information. Usage- At least one other status code is required to identify the missing or invalid information.;-Clm| Member ID (Loop 2010BA, NM109) is invalid. Invalid Data XGC000000M000-; [PE]
Member/Subscriber ID/Policy Number is invalid.
Resolution
Verify/Change the Insurance/Policy Number.
Sub-Element SV101-07
IT IS REQUIRED WHEN PROCEDURE CODE IS NON-SPECIFIC (SV101-02 IS J3301). SEGMENT SV1 IS DEFINED IN THE GUIDELINE AT POSITION 3.
The non-specific Procedure Code needs a more detailed description.
Resolution: Add a detailed description in the Note Field on the line item.
According to EDI, they move the info to the correct place
NOC (Not Otherwise Classified) codes need a description by Medicare standards.
Some Medicare replacements also require this.
This is sent in 2400 Loop.
Learn More: List of NOC Codes that Require a Description
Subscriber ID
- The claim was submitted to the incorrect Payer ID.
- Note: This is the most likely cause if this rejection was received on Claims for multiple patients.
- Resolution: Verify the Payer ID and modify if needed.
- The Patient’s demographics or Insurance Policy information included on the Claim was not eligible for the Date of Service billed.
- Verify the Patient's Eligibility.
- Verify the Patient's Name, DOB, and Policy Number.
- Resolution: Correct Patient demographics or Policy Information if it is incorrect.
- The Patient is a newborn or has been recently added to the Subscriber’s Insurance Policy.
- Resolution: Contact the Payer to verify the Patient's Policy status.
Learn More
Resubmit Claim
Zero Charge
PE: A6 - CHARGE MUST BE GREATER THAN ZERO [PE]
The Charge was sent with a $0.00 Fee.
The Payer does not accept $0.00.
Resolution: Three options for Resubmission
Enter a Fee for the Line Item/Charge.
Exclude the $0.00 Charge from the Claim.
If the Charge must be sent, enter $0.01 as the Fee Amount.
Related Articles
Payer Rejection Articles
Payer Rejections Payer Rejections Overview Acknowledgement/Receipt Payer Rejection: A6 -A1-;Acknowledgment/Receipt Adjudication Date Payer Rejected: INVALID ADJ PAYMENT DATE Claim Filing Indicator (CFI) Payer Rejection: INVALID FILING INDICATOR CODE ...Payment/Receipt FAQs
Adjustments/CARC Codes How can I post additional Adjustments? Post an Adjustment from: Payment Dashboard Patient Dashboard Encounter Dashboard Learn More Multiple Adjustment Lines Rebill the Claim from the Adjustment screen Adjustment Transaction ...Payer Rejection: INVALID FILING INDICATOR CODE 'CI'
PE: A6 PSBR0905-INVALID FILING INDICATOR CODE 'CI' PSBR0906-INVALID FILING INDICATOR CODE 'CI' The Claims Filing Indicator (CFI) is not correct. Resolution: Check the Claims Filing Indicator on the Insurance. Example: The CFI is CI (Commercial) in ...Charge/Claim FAQs
Charge/Claim FAQs Attachments How do I indicate there is attached paperwork? Attached Paperwork Attending Physician What is an Attending Physician? Attending Physician An Attending Physician is the one who is responsible for the overall care of a ...Add/Modify a Procedure Code (CPT)
CPT® Codes (Current Procedural Terminology) is a uniform medical language that defines the Procedures or Services performed by a qualified healthcare professional. They are referred to in the System as CPT or Procedure Codes. Adding fees directly to ...