Common Real-Time Eligibility Error Responses
Common Real-Time Eligibility Error Responses
You may receive a response that indicates Not Found/No Error Message Available or an Invalid/Rejection response.
- Some responses may indicate an issue on the Payer side.
Connection/High Volume Responses
- Not Found/No Error Message Available, Unable to Respond at Current Time, Please Correct and Resubmit
- Not Found/No Error Message Available with Exceptions, Unable to Respond at Current Time, Resubmission Allowed
- No Connection Available
- Possible Reasons
- This indicates that the Payer is unable to respond due to a connection issue on the Payers side or an EDI connection error.
- The Payer is receiving a high volume of requests.
- Retry your request later.
Missing/Invalid Subscriber/Insured ID
The following messages indicate that the Payer does not have a matching result in their System based on the information sent.
- Not Found/No Error Message Available, Subscriber/Insured Not Found, Please Correct and Resubmit
- Payer Rejected (Invalid), Invalid/Missing Subscriber/Insured Name. Please Correct and Resubmit
- Acknowledgement/Rejected for Invalid Information/Entity's contract/member number/Insured or Subscriber.
- Not Found/No Error Message Available, Patient Not Found. Please Correct and Resubmit
- Rejected/Review with Exceptions, Patient Birth Date Does Not Match for the Patient on the Database. (Most Commonly seen on Tricare Responses. For example, it was sent to Tricare East instead of Tricare for Life)
- Possible Reasons:
- Subscriber ID
- Group Number (if applicable)
- Patient First Name
- Patient Last Name
- Patient Middle Initial (if included on the Insurance Card)
- Patient Birthdate (DOB)
- Eligibility for submitted DOS
- Check the Patient's name, DOB, and Policy ID for accuracy.
- Verify that the correct Eligibility Payer ID is being used
- Some Payers have multiple Payer IDs based on the Patient's plan.
- Correct the Claim and resubmit.
Provider/NPI/Credentials
- Pending, Provider Not on File, Resubmission Not Allowed
- Cannot Process Invalid NPI
- Not Found/No Error Message Available, Authorization/Access Restrictions
- This could indicate that the NPI being used for this Payer is not valid (For example, the request is sent under the Group NPI, but the Provider is credentialed with the Payer as an Individual).
- Credentials being used for response are not valid.
- Reach out to Support for further assistance.
Medicare Responses
- Code: EMCHNL0020B - The number of eligibility requests sent to HETS for this Submitter ID, NPI, and MBI combination has exceeded CMS policy for today. (Source: E1)
- Medicare does not allow more than 3 invalid requests for a Patient and will not allow any additional requests for that day.
Miscellaneous Responses
- Contact Third Party
- Eligibility is not handled directly by this payer.
- Update the Policy's Payer ID with the appropriate Eligibility Payer ID.
- Select the Edit icon next to the Current Policy Holder.
- Select the Lookup icon next to Eligibility Payer ID.
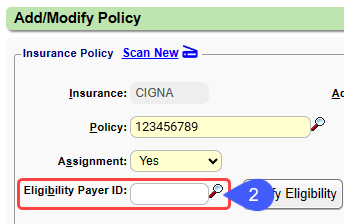
- Enter the Entity Name (found in the Eligibilty panel on the Eligibility Verification screen) and select the Eligibility Payer ID.
- After updating the Eligibility Payer ID, Eligibility must be verified again for the Status to update.

- If this does not resolve the issue, contact the Payer directly with the information given in the Eligibility Panel.
- Pending
- This is commonly seen for Medicare eligibility if hyphens are used in the policy ID.
- Remove the hyphens and retry the request.
- Non-ANSI Response: An unhandled error occurred running the real-time transaction
- An error has occurred.
- Reach out to Support for further assistance.
Related Articles
Real-Time Eligibility Verification
Insurance Eligibility can be checked from various locations in the System. The Eligibility Payer ID and Eligibility Time Frame is setup in the Insurance Library. Eligibility will reject if you have hyphens or any symbols in the Patient or Insurance ...Real-Time Claim Status
Real-Time Claim Status *This is a Premium Add-on feature. A Claim can appear to be Payer Accepted, but the Claim has not been adjudicated. The manual workflow to obtain a status on the Claim can be very time-consuming. Real-Time Claim Status (RTCS) ...Time Clock (Premium Add-On)
Time Clock/Card (Premium Add-On) This is a premium add-on feature. After your Practice is activated for the Time Card, you will need to enable it for each User in User Maintenance. The Clock icon can then be used to Clock In and Out and a Payroll ...Manually Add Eligibility Responses
There are times that a payer does not provide eligibility. The results obtained from a phone call or the Payer's web portal can be manually added. Select the Eligibility History link in the Active Policy panel on the Patient Dashboard. To manually ...Interactive Aging: Real-Time A/R View
The Interactive Aging Report is a real-time A/R Report. It can be grouped and aged dynamically. If the Bill Date is chosen as the Aging Date, and there is no Bill Date the System uses the Responsibility Date as the fallback date. This Report does not ...
